
Home / NCLEX-RN Practice Test Questions

NCLEX-RN Practice Test Questions
You've learned about the NCLEX-RN exam, studied the sections, and are ready to put your knowledge to the test. Take our practice NCLEX exam below to get ready for the real deal.
Jump to Section
Click on the section names below to jump to a particular section of the RegisteredNursing.org NCLEX-RN Practice Exam.
- The Safe and Effective Care Environment: The Management of Care
- The Safe and Effective Care Environment: Safety and Infection Control
- Health Promotion and Maintenance
- Psychosocial Integrity
- Physiological Integrity: Basic Care and Comfort
- Physiological Integrity: Pharmacological and Parenteral Therapies
- Physiological Integrity: Reduction of Risk Potential
- Physiological Integrity: Physiological Adaptation
The NCLEX-RN Test Plan is organized into four major Client Needs categories. Two of the four categories are divided into subcategories as shown below:
- Management of Care – 17% to 23%
- Safety and Infection Control – 9% to 15%
- Health Promotion and Maintenance – 6% to 12%
- Psychosocial Integrity – 6% to 12%
- Basic Care and Comfort – 6% to 12%
- Pharmacological and Parenteral Therapies – 12% to 18%
- Reduction of Risk Potential – 9% to 15%
- Physiological Adaptation – 11% to 17%
For more practice test questions from professional sources try these .

The Safe & Effective Care Environment: The Management of Care Practice Questions
You should respond to the couple by stating that only unanticipated treatments and procedures that are not included in the advance directive can be made by the legally appointed durable power of attorney for healthcare decisions.
- You should be aware of the fact that the wife of the client has a knowledge deficit relating to advance directives and durable powers of attorney for healthcare decisions and plan an educational activity to meet this learning need.
- You should be aware of the fact that the client has a knowledge deficit relating to advance directives and durable powers of attorney for healthcare decisions and plan an educational activity to meet this learning need.
- You should reinforce the wife’s belief that legally married spouses automatically serve for the other spouse’s durable power of attorney for health care decisions and that others than the spouse cannot be legally appointed while people are married
Correct Response: A
Both the client and the client’s spouse have knowledge deficits relating to advance directives. Legally married spouses do not automatically serve for the other spouse’s durable power of attorney for health care decisions; others than the spouse can be legally appointed while people are married.
- Privacy and to have their medical information confidential unless the client formally approves the sharing of this information with others such as family members.
- Make healthcare decisions and to have these decisions protected and communicated to others when they are no longer competent to do so.
- Be fully informed about all treatments in term of their benefits, risks and alternatives to them so the client can make a knowledgeable and informed decision about whether or not to agree to having it
- Make decisions about who their health care provider is without any coercion or undue influence of others including healthcare providers.
Correct Response: B,D
The Patient Self Determination Act, which was passed by the US Congress in 1990, gives Americans the right to make healthcare decisions and to have these decisions protected and communicated to others when they are no longer competent to do so. These decisions can also include rejections for future care and treatment and these decisions are reflect in advance directives. This Act also supports the rights of the client to be free of any coercion or any undue influence of others including healthcare providers.
The Health Insurance Portability and Accountability Act (HIPAA) supports and upholds the clients’ rights to confidentially and the privacy of their medical related information regardless of its form. It covers hard copy and electronic medical records unless the client has formally approved the sharing of this information with others such as family members.
The elements of informed consent which includes information about possible treatments and procedures in terms of their benefits, risks and alternatives to them so the client can make a knowledgeable and informed decision about whether or not to agree to having it may be part of these advanced directives, but the law that protects these advance directives is the Patient Self Determination Act.
- Call the doctor and advise them that the client’s physical status has significantly changed and that they have just had a cardiopulmonary arrest.
- Begin cardiopulmonary resuscitation other emergency life saving measures.
- Notify the family of the client’s condition and ask them what they should be done for the client.
- Insure that the client is without any distressing signs and symptoms at the end of life.
Correct Response: B
You must immediately begin cardiopulmonary resuscitation and all life saving measures as requested.by the client in their advance directive despite the nurse’s own beliefs and professional opinions. Nurses must uphold the client’s right to accept, choose and reject any and all of treatments, as stated in the client’s advance directive.
You would not call the doctor first; your priority is the sustaining of the client’s life; you would also not immediately notify the family for the same reason and, when you do communicate with the family at a later time, you would not ask them what should or should not be done for the client when they wishes are already contained in the client’s advance directive.
Finally, you would also insure that the client is without pain and all other distressing signs and symptoms at the end of life, but the priority and the first thing that you would do is immediately begin cardiopulmonary resuscitation and all life saving measures as requested by the client in their advance directive, according to the ABCs and Maslow’s Hierarchy of Needs.
- Case manager
- Collaborator
- Coordinator of care
Correct Response: D
The priority role of the nurse is advocacy. The nurse must serve as the advocate for both the fetus and the mother at risk as the result of this ethical dilemma where neither option is desirable. As an advocate, the nurse would seek out resources and people, such as the facility’s ethicist or the ethics committee, to resolve this ethical dilemma.
- Client advocate
- Entrepreneur
A nurse who organizes and establishes a political action committee (PAC) in their local community to address issues relating to the accessibility and affordability of healthcare resources in the community is serving as the client advocate. As you should know, the definition of “client” includes not only individual clients, and families as a unit, but also populations such as the members of the local community.
Although the nurse, as the organizer of this political action committee (PAC), will have to collaborate with members of the community to promote the accessibility and affordability of healthcare resources in the community, this is a secondary role rather than the primary role.
Additionally, although the nurse is serving in a political advocacy effort, the nurse is not necessarily a politician and there is no evidence that this nurse is an entrepreneur.
- The right task, the right circumstances, the right person, the right competency, and the right supervision or feedback
- The right task, the right circumstances, the right person, the right direction or communication, and the right supervision or feedback
- The right competency, the right education and training, the right scope of practice, the right environment and the right client condition
- The right competency, the right person, the right scope of practice, the right environment and the right client condition
The Five Rights of Delegation include the right task, the right circumstances, the right person, the right direction or communication, and the right supervision or feedback.
The right competency is not one of these basic Five Rights, but instead, competency is considered and validated as part of the combination of matching the right task and the right person; the right education and training are functions of the right task and the right person who is able to competently perform the task; the right scope of practice, the right environment and the right client condition are functions of the legal match of the person and the task; and the setting of care which is not a Right of Delegation and the matching of the right person, task and circumstances.
- The American Nurses Association’s Scopes of Practice
- The American Nurses Association’s Standards of Care
- State statutes
- Federal law
Correct Response: C
The registered nurse, prior to the delegation of tasks to other members of the nursing care team, evaluates the ability of staff members to perform assigned tasks for the position as based on state statutes that differentiate among the different types of nurses and unlicensed assistive personnel that are legally able to perform different tasks.
Although the American Nurses Association’s Standards of Care guide nursing practice, these standards are professional rather than legal standards and the American Nurses Association does not have American Nurses Association’s Scopes of Practice, only the states’ laws or statutes do.
Lastly, scopes of practice are within the legal domain of the states and not the federal government.
- Observe the staff member during an entire shift of duty to determine whether or not the nurse has accurately and appropriately established priorities.
- Observe the staff member during an entire shift of duty to determine whether or not the nurse has accurately and appropriately completed priority tasks.
- Ask the staff member how they feel like they have been able to employ their time management skills for the last six months.
- Collect outcome data over time and then aggregate and analyze this data to determine whether or not the staff member has completed reasonable assignments in the allotted time before the end of their shift of duty.
The best way to objectively evaluate the effectiveness of an individual staff member’s time management skills in a longitudinal manner is to collect outcome data over time, and then aggregate and analyze this data to determine whether or not the staff member has completed reasonable assignments in the allotted time before the end of their shift of duty. Another way to perform this longitudinal evaluation is to look at the staff member’s use of over time, like the last six months, when the unit was adequately staffed.
Observing the staff member during an entire shift of duty to determine whether or not the nurse has accurately and appropriately established priorities is a way to evaluate the short term abilities for establishing priorities and not assignment completion and observing the staff member during an entire shift of duty to determine whether or not the nurse has accurately and appropriately completed priority tasks is a way to evaluate the short term abilities for completing established priorities and not a complete assignment which also includes tasks that are not of the highest priority.
Lastly, asking the staff member how they feel like they have been able to employ their time management skills for the last six months is the use of subjective rather than objective evaluation.
- An unlicensed staff member who has been “certified” by the employing agency to monitor telemetry: Monitoring cardiac telemetry
- An unlicensed assistive staff member like a nursing assistant who has been “certified” by the employing agency to insert a urinary catheter: Inserting a urinary catheter
- A licensed practical nurse: The circulating nurse in the perioperative area
- A licensed practical nurse: The first assistant in the perioperative area
An unlicensed staff member who has been “certified” by the employing agency to monitor telemetry can monitor cardiac telemetry; they cannot, however, interpret these cardiac rhythms and initiate interventions when interventions are indicated. Only the nurse can perform these roles.
Unlicensed assistive staff member like a nursing assistant cannot under any circumstances be certified” by the employing agency to insert a urinary catheter or insert a urinary catheter because this is a sterile procedure and, legally, no sterile procedures can be done by an unlicensed assistive staff member like a nursing assistant.
Lastly, the role of the circulating nurse is within the exclusive scope of practice for the registered nurse and the role of the first assistant is assumed only by a registered nurse with the advanced training and education necessary to perform competently in this capacity. Neither of these roles can be delegated to a licensed practical nurse or an unlicensed assistive staff member like a nursing assistant or a surgical technician.
- Only the VA health care services because he is not 65 years of age
- Medicare because he has been deemed permanently disabled for 2 years
- Medicaid because he is permanently disabled and not able to work
- Choices B and C
This client is legally eligible for Medicare because he has been deemed permanently disabled for more than 2 years in addition to the VA health care services. People over the age of 65 and those who are permanently disabled for at least two years, according to the Social Security Administration, are eligible for Medicare.
Based on the information in this scenario, the client is not eligible for Medicaid because has a “substantial” VA disability check on a monthly basis and is not indigent and with a low income.
- The case manager’s role in terms of organization wide performance improvement activities
- The case manager’s role in terms complete, timely and accurate documentation
- The case manager’s role in terms of the clients’ being at the appropriate level of care
- The case manager’s role in terms of contesting denied reimbursements
Registered nurse case managers have a primary case management responsibility associated with reimbursement because they are responsible for insuring that the client is being cared for at the appropriate level of care along the continuum of care that is consistent with medical necessity and the client’s current needs. A failure to insure the appropriate level of care jeopardizes reimbursement. For example, care in an acute care facility will not be reimbursed when the client’s current needs can be met in a subacute or long term care setting.
Nurse case managers do not have organization wide performance improvement activities, the supervision of complete, timely and accurate documentation or challenging denied reimbursements in their role. These roles and responsibilities are typically assumed by quality assurance/performance improvement, supervisory staff and medical billers, respectively.
- The ProACT Model: Registered nurses perform the role of the primary nurse in addition to the related coding and billing functions
- The Collaborative Practice Model: The registered nurse performs the role of the primary nurse in addition to the role of the clinical case manager with administrative, supervisory and fiscal responsibilities
- The Case Manager Model: The management and coordination of care for clients throughout a facility who share the same DRG or medical diagnosis
- The Triad Model of Case Management: The joint collaboration of the social worker, the nursing case manager, and the utilization review team
The Triad Model of case management entails the joint collaboration of the social worker, the nursing case manager, and the utilization review team.
The Professionally Advanced Care Team, referred to as the ProACT Model, which was developed at the Robert Wood Johnson University Hospital, entails registered nurses serving in the role of both the primary nurse the clinical case manager with no billing and coding responsibilities; these highly specialized and technical billing and coding responsibilities are done by the business office, medical billers and medical coders.
The Case Manager Model entails the registered nurses’ role in terms of case management for a particular nursing care unit for a group of clients with the same medical diagnosis or DRG. In contrast to this Case Manager Model of Beth Israel Hospital, the Collaborative Practice Model of case management entails the role of some registered nurses in a particular healthcare facility to manage, coordinate, guide and direct the complex care of a population of clients throughout the entire healthcare facility who share a particular diagnosis or Diagnostic Related Group.
- The Case Manager Model
- The ProACT Model
- The Collaborative Practice Model
- The Triad Model of Case Management
The Case Manager Model and the Collaborative Practice Model of case management are the only models of case management that employ the mandated and intrinsic use of critical pathways which are multidisciplinary plans of care that are based on the client’s current condition, and that reflect interventions and expected outcomes within a pre-established time line.
The ProACT Model, the Collaborative Practice Model and the Triad Model of Case Management do not necessarily employ critical pathways; these models can use any system of medical records and documentation.
- An opt out consent
- An implicit consent
- An explicit consent
- No consent at all is given
The type of legal consent that is indirectly given by the client by the very nature of their voluntary acute care hospitalization is an implicit consent indirectly given by the client by the very nature of their voluntary acute care hospitalization is an implicit consent.
An explicit consent, on the other hand, is the direct and formal consent of the client; and an opt out consent is given when a patient does NOT refuse a treatment; this lack of objections by the patient indicates that the person has consented to the treatment or procedure with an opt out consent.
- Take the photographs because these photographs are part of the holiday tradition at this facility
- Take the photographs because all of the residents are properly attired and in a dignified condition
- Refuse to take the photographs unless you have the consent of all to do so
- Refuse to take the photographs because this is not part of the nurse’s role
You should refuse to take the photographs unless you have the consent of all to do so because to do otherwise is a violation of the residents’ rights to privacy and confidentiality as provided in the Health Insurance Portability and Accountability Act (HIPAA). This, rather than the false belief that this is not part of the nurse’s role, is the reason that you would not automatically take these photographs.
Regardless of whether or not these photographs are part of the holiday tradition at this facility and whether or not the residents are properly attired and in a dignified condition, no photographs can be legally taken without the residents’ permission and consent.
- The Patient Self Determination Act: The client’s right to choose the level of care
- The Patient Self Determination Act: The clients’ right to healthcare insurance coverage for mental health disorders
- The Mental Health Parity Act: The privacy and security of technological psychiatric information
- The Health Insurance Portability and Accountability Act (HIPAA): The privacy and security of technological medical information
The Health Insurance Portability and Accountability Act (HIPAA) protects the client’s legal rights to the privacy, security and confidentiality of all medical information including data and information that is technologically stored and secured.
The Patient Self Determination Act uphold the client’s right to choose and reject care and not the level of care that is driven and decided upon as based on medical necessity and health insurance reimbursement; this Act also does not give client’s the right to any health insurance including healthcare insurance coverage for mental health disorders.
Lastly, the Mental Health Parity and Addiction Equality Act, passed in 2008, mandates insurance coverage for mental health and psychiatric health services in a manner similar to medical and surgical insurance coverage; it does not protect the privacy and security of technological psychiatric information, HIPAA does.
- The physical therapist
- The occupational therapist
- The podiatrist
- The nurse practitioner
The member of the multidisciplinary team that you would most likely collaborate with when the client is at risk for falls due to an impaired gait is a physical therapist. Physical therapists are licensed healthcare professionals who assess, plan, implement and evaluate interventions including those related to the patient’s functional abilities in terms of their gait, strength, mobility, balance, coordination, and joint range of motion. They also provide patients with assistive aids like walkers and canes and exercise regimens.
Occupational therapists assess, plan, implement and evaluate interventions including those that facilitate the patient’s ability to achieve their highest possible level of independence in terms of their activities of daily living such as bathing, grooming, eating and dressing.
Podiatrists care for disorders and diseases of the foot; and nurse practitioners, depending on their area of specialty, may also collaborate with nurses when a client is affected with a disorder in terms of gait, strength, mobility, balance, coordination, and joint range of motion, however the member of the multidisciplinary team that you would most likely collaborate with when the client is at risk for falls due to an impaired gait is a physical therapist.
- The dietician
The member of the multidisciplinary team that you would most likely collaborate with when the client can benefit from the use of adaptive devices for eating is the occupational therapist. Occupational therapists assess, plan, implement and evaluate interventions including those that facilitate the patient’s ability to achieve their highest possible level of independence in terms of their activities of daily living such as bathing, grooming, eating and dressing. Many of these interventions include adaptive devices such as special eating utensils and grooming aids.
Physical therapists are licensed healthcare professionals who assess, plan, implement and evaluate interventions including those related to the patient’s functional abilities in terms of their gait, strength, mobility, balance, coordination, and joint range of motion. They also provide patients with assistive aids like walkers and canes and exercise regimens.
Dieticians assess, plan, implement and evaluate interventions including those relating to dietary needs of those patients who need regular or therapeutic diets. They also provide dietary education and work with other members of the healthcare need when a client has dietary needs secondary to physical disorders such as dysphagia; and podiatrists care for disorders and diseases of the foot.
- To fulfill the nurse’s role in terms of collaboration
- To plan and provide for optimal client outcomes
- To solve complex multidisciplinary patient care problems
- To provide educational experiences for experienced nurses
The primary goal of multidisciplinary case conferences is to plan care that facilitates optimal client outcomes. Other benefits of multidisciplinary case conferences include the fulfillment of the nurse’s role in terms of collaboration and collegiality, to solve complex multidisciplinary patient care problems so that optimal client outcomes can be achieved and also to provide educational experiences for nurses; these things are secondary rather than primary goals.
- A Pedorthist
- A pediatric nurse practitioner
- A trauma certified clinical nurse specialist
- A prosthetist
The member of the multidisciplinary team would you most likely collaborate with when your pediatric client has had a traumatic amputation secondary to a terrorism blast explosion a month ago or more ago is a prosthetist. Prosthetists, in collaboration with other members of the healthcare team, assess patients and then design, fit and supply the patient with an artificial body part such as a leg or arm prosthesis. They also follow-up with patients who have gotten a prosthesis to check and adjust it in terms of proper fit, patient comfort and functioning.
Pedorthists modify and provide corrective footwear and employ supportive devices to address conditions which affect the feet and lower limbs. Lastly, you may collaborate with a trauma certified clinical nurse specialist and a pediatric nurse practitioner but this consultation and collaboration should begin immediately upon arrival to the emergency department, and not a month after the injury.
- Conceptualization conflicts
- Avoidance - Avoidance conflicts
- Approach - Approach conflicts
- Resolvable conflicts
- Unresolvable conflicts
- Double Approach - Avoidance conflicts
- Approach-Avoidance conflicts
Correct Response: B, C, F, G
According to Lewin, the types of conflict are Avoidance-Avoidance conflicts, Approach- Approach conflicts, Double Approach - Avoidance conflicts and Approach-Avoidance conflicts.
- Frustration: The phase of conflict that is characterized with personal agendas and obstruction
- Conceptualization: The phase of conflict that occurs when contending parties have developed a clear and objective understanding of the nature of the conflict and factors that have led to it
- Taking action: The phase of conflict that is characterized with individual responses to and feelings about the conflict
- Resolution: The type of conflict that can be resolved
- Avoidance-Avoidance: A stage of conflict that occurs when there are NO alternatives that are acceptable to the contending parties
- Approach- Approach Conflicts: The type of conflict that occurs when the people involved in the conflict want more than one alternatives or actions that could resolve the conflict.
- Approach-Avoidance Conflicts: The type of conflict that occurs when the people involved in the conflict believe that all of the alternatives are NEITHER completely satisfactory nor completely dissatisfactory.
Correct Response: C, F, G
Taking action is the phase of conflict that is characterized with individual responses to and feelings about the conflict; Approach- Approach conflicts are a type of conflict that occurs when the people involved in the conflict want more than one alternatives or actions that could resolve the conflict; and Approach-Avoidance conflicts are a type of conflict that occurs when the people involved in the conflict believe that all of the alternatives are NEITHER completely satisfactory or completely dissatisfactory.
Frustration is the phase of conflict that occurs when those involved in the conflict believe that their goals and needs are being blocked and not met, and not necessarily characterized with personal agendas and obstruction; conceptualization is the phase of conflict that occurs when those involved in the conflict begin to understand what the conflict is all about and why it has occurred. This understanding often varies from person to person and this personal understanding may or may not be accurate, clear or objective, and not a clear and objective understanding of the nature of the conflict and factors that have led to it; resolution is a phase of conflict resolution, not a type of conflict, that is characterized when the contending parties are able to come to some agreement using mediation, negotiation or another method; an Avoidance-Avoidance conflict is a type of conflict and not a phase of conflict, that occurs when there are NO alternatives that are acceptable to any the contending parties; Approach- Approach conflicts occur when the people involved in the conflict want more than one alternative or action that could resolve the conflict; and lastly, Double Approach - Avoidance is a type of conflict and not a stage of conflict that occurs when the people involved in the conflict are forced to choose among alternatives and actions, all of which have BOTH positive and negative aspects to them.
- Competition
- Accommodating Others
Conflicts can be effectively resolved using a number of different strategies and techniques such as compromise, negotiation, and mediation.
Avoidance of the conflict, withdrawing in addition to other passivity, competition, and accommodating others are not effective and healthy conflict resolution techniques.
- Conceptualization
- Frustration
- Taking action
Correct Response: B, A, D, C
The stages of conflict and conflict resolution in the correct sequential order are frustration, conceptualization, and taking action.
- The Patient Self Determination Act
- The Mental Health Parity Act
- The Health Insurance Portability and Accountability Act
- The Americans with Disabilities Act of 1990
The federal law is most closely associated with the highly restrictive “need to know” is the Health Insurance Portability and Accountability Act. This law restricts access to medical information to only those persons who have the need to know this information in order to provide direct and/or indirect care to the client.
The Mental Health Parity Act passed in 2008, mandates insurance coverage for mental health and psychiatric health services in a manner similar to medical and surgical insurance coverage.
And, lastly the Americans with Disabilities Act of 1990 and the Rehabilitation Act of 1973 forbid and prohibit any discrimination against people with disabilities.
- The facility’s Performance Improvement Director who is not a healthcare person and who has no direct contact with clients
- A nursing student who is caring for a client under the supervision of the nursing instructor
- The facility’s Safety Officer who is not a healthcare person and who has no direct contact with clients
- A department supervisor with no direct or indirect care duties
A department supervisor with no direct or indirect care duties does not have the “right to know” medical information; all of the others have the “right to know” medical information because they provide direct or indirect care to clients.
For example, both the facility’s Performance Improvement Director who is not a healthcare person and who has no direct contact with clients and the facility’s Safety Officer who is not a healthcare person and who has no direct contact with clients provide indirect care to clients. For example, they collect and analyze client data in order to fulfill their role and responsibilities in terms of process improvements and the prevention of incidents and accidents, respectively.
Nursing and other healthcare students also have the “need to know” medical information so that they can provide direct client care to their assigned client(s).
- “A computer in the hallway was left unattended and a client’s medical record was visible to me.”
- “I just saw a nursing student looking at the medical record for a client that they are NOT caring for during this clinical experience.”
- “As I was walking past the nursing station, I saw a dietician reading the progress notes written by members of the laboratory department in addition to other dieticians’ progress notes.”
- “I refused the nursing supervisor’s request to share my electronic password for the new nurse on the unit.”
A staff members comment, “As I was walking past the nursing station, I saw a dietician reading the progress notes written by members of the laboratory department in addition to other dieticians’ progress notes” “indicates the need for the Nurse Manager to provide an educational activity relating to confidentiality and information security because dieticians often have the “need to know” about laboratory data so that they can, for example, assess the client’s nutritional status in terms of their creatinine levels.
The report that the nursing student was “looking at the medical record for a client that they are NOT caring for during this clinical experience” indicates that the reporting staff member is correctly applying the principles for maintaining confidentiality and privacy of information; the report that a “computer in the hallway was left unattended and a client’s medical record was visible to me” indicates that the reporting staff member is correctly applying the principles for maintaining confidentiality and privacy of information; and lastly, “I refused the nursing supervisor’s request to share my electronic password for the new nurse on the unit” also indicates that the staff member is knowledgeable about privacy and confidentiality.
- Case management
- Continuity of care
- Medical necessity
- Critical pathway
The continuity of care is defined as the sound, timely, smooth, unfragmented and seamless transition of a client from one area within the same healthcare facility, from one level of care to a higher and more intense level of care or to a less intense level of care based on the client’s status and level of acuity, from one healthcare facility to another healthcare facility and also any discharges to the home in the client’s community.
Case management and critical pathways may be used to facilitate the continuity of care, but they are not the sound, timely, smooth, unfragmented and seamless transition of the client from one level of acuity to another. Lastly, medical necessity is necessary for reimbursement and it is one of the considerations for moving the client from one level of acuity to another but medical necessity is not the continuity of care.
- The Four P's
The standardized “hand off” change of shift reporting system that you may want to consider for implementation on your nursing care unit is ISBAR. Other standardized change of shift “hand off” reports, as recommended by the Joint Commission on the Accreditation of Healthcare Organization, include:
- SBAR, not IBAR
- The Five Ps not the Four Ps and
Lastly, MAUUAR is a method of priority setting and not a standardized “hand off” change of shift reporting system.
- SBAR: Symptoms, background, assessment and recommendations
- ISBAR: Interventions, symptoms, background, assessment and recommendations
- The Five Ps: The patient, plan, purpose, problems and precautions
- BATON: Background, assessment, timing, ownership and next plans
The Five Ps are the patient, plan, purpose, problems and precautions.
The elements of the other standardized reporting systems are listed below:
SBAR stands for:
- S: Situation: The patient’s diagnosis, complaint, plan of care and the patient's prioritized needs
- B: Background: The patient’s code or DNR status, vital Signs, medications and lab results
- A: Assessment: The current assessment of the situation and the patient’s status and
- R: Recommendations: All unresolved issues including things like pending diagnostic testing results and what has to be done over the next few hours
ISBAR stands for:
- I: Introduction: The introduction of the nurse, the nurse’s role in care and the area or department that you are from
- R: Recommendations: All unresolved issues including things like pending diagnostic testing results and what has to be done over the next few hours
BATON stands for:
- B: Background: Past and current medical history, including medications
- A: Actions: What actions were taken and/or those actions that are currently required
- T: Timing: Priorities and level of urgency
- O: Ownership: Who is responsible for what? and
- N: Next: The future plan of care
IPASS stands for:
- I ntroduction: The introduction of the nurse, the nurse’s role in care and the area or department that you are from
- P: Patient: The patient’s name, age, gender, location and other demographic data
- A: Assessment: The current assessment of the situation and the patient’s status
- S: Situation: The patient’s diagnosis, complaint, plan of care and the patient's prioritized needs and
- S: Safety concerns: Physical, mental and social risks and concerns
- Atrial fibrillation
- First degree heart block
- Shortness of breath upon exertion
- An obstructed airway
- Fluid needs
- Respect and esteem by others
- 3,4,2,1,5,6
- 3,4,5,1,2,6
- 2,3,5,1,4,6
- 3,2,4,1,5,6
Correct Response:
Client needs are prioritized in a number of different ways including Maslow’s Hierarchy of Human Needs and the ABCs. In terms of priorities from # 1 to # 6 the conditions above are prioritized as follows:
The ABCs identifies the airway, breathing and cardiovascular status of the patient as the highest of all priorities in that sequential order; and Maslow’s Hierarchy of Needs identifies the physiological or biological needs, including the ABCs, the safety/psychological/emotional needs, the need for love and belonging, the needs for self-esteem and the esteem by others and the self-actualization needs in that order of priority.
- Understanding level
One of the 2 nd priority needs according to the MAAUAR method of priority setting is risks.
The ABCs / MAAUAR method of priority setting places the ABCs, again, as the highest and greatest priorities which are then followed with the 2 nd and 3 rd priority level needs of the MAAUAR method of priority setting.
The 2 nd priority needs according to the MAAUAR method of priority setting after the ABCs include M-A-A-U-A-R which stands for:
- M ental status changes and alterations
- A cute pain
- A cute urinary elimination concerns
- U naddressed and untreated problems that require immediate priority attention
- A bnormal laboratory and other diagnostic data that are outside of normal limits and
- R isks including those relating to a healthcare problem like safety, skin breakdown, infection and other medical conditions
The 3 rd level priorities include all concerns and problems that are NOT covered under the 2 nd level priority needs and the ABCs. For example, increased levels of self care abilities and skills and enhanced knowledge of a medical condition are considered 2 nd level priority needs.
- Time management skills
- Communication skills
- Collaboration skills
- Supervision skills
Time management skills are most closely related to successfully meeting the established priority needs of a group of clients.
In addition to prioritizing and reprioritizing, the nurse should also have a plan of action to effectively manage their time; they should avoid unnecessary interruptions, time wasters and helping others when this helping others could potentially jeopardize their own priorities of care.
Although good communication skills, collaboration skills and supervision are necessary for the delivery of nursing care, it is time management skills that are most closely related to successfully meeting the established priority needs of a group of clients.
- Client rights
Morals are most closely aligned with ethics. Ethics is a set of beliefs and principles that guide us in terms of the right and wrong thing to do which is the most similar to ethics.
Laws and statutes defined what things are legal and what things are illegal. Lastly, client rights can serve as a factor to consider when ethical decisions are made; but they are not most closely aligned with ethics, but only, one consideration of many that can be used in ethical decision making.
- Deontology: The school of ethical of thought that requires that only the means to the goal must be ethical.
- Utilitarianism: The school of ethical of thought that requires that only the end goal must be ethical.
- Deontology: The school of ethical of thought that requires that only the end goal must be ethical.
- Utilitarianism: The school of ethical of thought that requires that only the means to the goal must be ethical.
The two major classifications of ethical principles and ethical thought are utilitarianism and deontology. Deontology is the ethical school of thought that requires that both the means and the end goal must be moral and ethical; and the utilitarian school of ethical thought states that the end goal justifies the means even when the means are not moral.
- Justice: Equally dividing time and other resources among a group of clients
- Beneficence: Doing no harm during the course of nursing care
- Veracity: Fully answering the client’s questions without any withholding of information
- Fidelity: Upholding the American Nurses Association’s Code of Ethics
Fully answering the client’s questions without any withholding of information is an example of the application of veracity into nursing practice. Veracity is being completely truthful with patients; nurses must not withhold the whole truth from clients even when it may lead to patient distress.
Justice is fairness. Nurses must be fair when they distribute care and resources equitably, which is not always equally among a group of patients. Beneficence is doing good and the right thing for the patient; it is nonmaleficence that is doing no harm.
- Planning a way to evaluate the effectiveness of the class by seeing a decrease in the amount of referrals to the facility’s Ethics Committee
- Establishing educational objectives for the class that reflect the methods and methodology that you will use to present the class content
- The need to exclude case studies from the class because this would violate client privacy and confidentiality
- Some of the most commonly occurring bioethical concerns including genetic engineering into the course content
You would consider including some of the most commonly occurring bioethical concerns including genetic engineering into the course content.
You would also plan how you could evaluate the effectiveness of the class by seeing an increase, not a decrease in the amount of referrals to the facility’s Ethics Committee, because one of the elements of this class should address ethical dilemmas and the role of the Ethics Committee in terms of resolving these.
You would additionally establish educational objectives for the class that reflect specific, measurable learner outcomes and not the methods and methodology that you will use to present the class content; and lastly, there is no need to exclude case studies from the class because “sanitized” medical records can, and should be, used to avoid any violations of client privacy and confidentiality.
- Serve as the witness to the client’s signature on an informed consent.
- Get and witness the client’s signature on an informed consent.
- Get and witness the durable power of attorney for health care decisions’ signature on an informed consent.
- None of the above
One of the roles of the registered nurse in terms of informed consent is to serve as the witness to the client’s signature on an informed consent.
Other roles and responsibilities of the registered nurse in terms of informed consent include identifying the appropriate person to provide informed consent for client, such as the client, parent or legal guardian, to provide written materials in client’s spoken language, when possible, to know and apply the components of informed consent, and to also verify that the client comprehends and consents to care and procedures.
The registered nurse does not get the client’s or durable power of attorney for health care decisions’ signature on an informed consent, this is the role and responsibility of the physician or another licensed independent practitioner.
- Self determination
- Nonmalficence
Self-determination is most closely aligned with the principles and concepts of informed consent. Self-determination supports the client’s right to choose and reject treatments and procedures after they have been informed and fully knowledgeable about the treatment or procedure.
Justice is fairness. Nurses must be fair when they distribute care and resources equitably, which is not always equally among a group of patients; fidelity is the ethical principle that requires nurses to be honest, faithful and true to their professional promises and responsibilities by providing high quality, safe care in a competent manner; and, lastly, nonmaleficence is doing no harm, as stated in the historical Hippocratic Oath.
- The purpose of the proposed treatment or procedure
- The expected outcomes of the proposed treatment or procedure
- Who will perform the treatment or procedure
- When the procedure or treatment will be done
The minimal essential components of the education that occurs prior to getting an informed consent include the purpose of the proposed treatment or procedure, the expected outcomes of the proposed treatment or procedure, and who will perform the treatment or procedure. It is not necessary to include when the treatment or procedure will be done at this time.
Other essential elements include:
- The benefits of the proposed treatment or procedure
- The possible risks associated with the proposed treatment or procedure
- The alternatives to the particular treatment or procedure
- The benefits and risks associated with alternatives to the proposed treatment or procedure
- The client’s right to refuse a proposed treatment or procedure
- The Security Rule
- The American Nurses Association’s Code of Ethics
- The American Hospital’s Patients’ Bill of Rights
- The Autonomy Rule
Prohibitions against sharing passwords are legally based on the Security Rule of HIPAA mandates administrative, physical, and technical safeguards to insure the confidentiality, integrity, and availability of electronic protected health information. This rule relates to electronic information security as well as other forms of information.
The American Nurses Association’s Code of Ethics and the American Hospital’s Patients’ Bill of Rights both address client confidentiality and their rights to privacy, however, these statements are not legal, but instead ethical and regulatory statements; and lastly, there is no autonomy law or rule.
- Social networks and cell phone cameras pose low risk in terms of information technology security and confidentiality.
- The security of technological data and information in healthcare environments is most often violated by those who work there.
- The security of technological data and information in healthcare environments is most often violated by computer hackers.
- Computer data deletion destroys all evidence of the data.
The security of technological data and information in healthcare environments is most often violated by those who work there. The vast majority of these violations occur as the result of inadvertent breaches with carelessness and the lack of thought on the part of employees. Technology is a double edged sword.
Technological advances such as cell phone cameras, social networks like Facebook, telephone answering machines and fax machines pose great risk in terms of the confidentiality and the security of medical information. Computer data deletion does not always destroy all evidence of the data; data remains.
- Assault: Touching a person without their consent
- Battery: Threatening to touch a person without their consent
- Slander: False oral defamatory statements.
- Slander: False written defamatory statements.
Slander is false oral defamatory statements; and libel is written defamation of character using false statements.
Assault, an intentional tort, is threatening to touch a person without their consent; and battery, another intentional tort, is touching a person without their consent.
- Ensured the client’s safety which is a high patient care priority
- Violated Respondeat Superior
- Violated the client’s right to dignity
- Committed a crime
When you loosely apply a bed sheet around your client’s waist to prevent a fall from the chair, you have falsely imprisoned the client with this make shift restraint. False imprisonment is restraining, detaining and/or restricting a person’s freedom of movement. Using a restraint without an order is considered false imprisonment even when it is done to protect the client’s safety.
Respondeat Superior is the legal doctrine or principle that states that employers are legally responsible for the acts and behaviors of its employees. Respondeat Superior does not, however, relieve the nurse of legal responsibility and accountability for their actions. They remain liable.
There is no evidence in this question that you have violated the client’s right to dignity.
- Respondeat Superior does not mean that a nurse cannot be held liable.
- Respondeat Superior does not mean that a nurse cannot be held libel.
- Respondeat Superior is an ethical principle.
- Respondeat Superior is a law.
Respondeat Superior does not mean that a nurse cannot be held liable and not libel which is a written defamation of character using false statements. Liability is legal vulnerability.
Respondeat Superior is the legal doctrine or principle and not a law or ethical principle.
- Causation, foreseeability, damages to the patient, a duty that was owed to the client and this duty was breached, and direct rather than indirect harm to the client.
- Causation, foreseeability, damages to the patient, a duty that was owed to the client and this duty was breached, and direct and/or indirect harm to the client.
- Causation, correlation, damages to the patient, a duty that was owed to the client and this duty was breached, and direct and/or indirect harm to the client.
- Causation, foreseeability, damages to the patient, a duty that was owed to the client and this duty was breached, and a medical license.
The six essential components of malpractice include causation, foreseeability, damages to the patient, a duty that was owed to the client and this duty was breached, and, lastly, this breach of duty led to direct and/or indirect harm to the client.
A medical license is not necessary; nurses and other healthcare professionals can be found guilty of malpractice. Lastly, correlation is the relationship of simultaneously changing variables. For example, a ppositive correlation exists when the two variables both increase or decrease; and a negative occurs when one variable increases and the other decreases.
- Sound structures like policies and procedures
- Processes and how they are being done
- Optimal client outcomes
- Optimal staff performance
The current focus of performance improvement activities is to facilitate and address optimal client outcomes. Throughout the last several decades performance improvement activities have evolved from a focus on structures to a focus on process and now, to a focus on outcomes.
Staff performance is not the focus of performance improvement activities but instead the focus of competency assessment and validation.
- An adverse event
- A root cause
- A healthcare acquired event
- A sentinel event
A sentinel event is an event or occurrence, incident or accident that has led to or may have possibly led to client harm. Even near misses, that have the potential for harm, are considered sentinel events because they have the potential to cause harm in the future.
An adverse event, like an adverse effect of a medication, has actually led to an adverse response; it is not a near miss. A root cause is a factor that has led to a sentinel event; and there is no such thing as a healthcare acquired event.
- Discover a process flaw
- Determine who erred
- Discover environmental hazards
- Determine basic client needs
The primary purpose of root cause analysis is to discover process flaws. Root cause analysis and a blame free environment are essential to a successful performance improvement activity, therefore, root cause analysis does not aim to determine who erred and made a mistake. Root cause analysis explores and digs down to the roots of the problem, its root causes and the things, not people, which are the real reasons why medical errors and mistakes are made.
It is nursing assessment that determines the basic client needs and environmental surveillance that discovers environmental safety hazards, and not root cause analysis.
Root cause analysis activities ask “Why”, rather than “Who”, which would place blame on a person or group of people: and What? and When? Questions are rarely asked.
- Historical data and performance improvement activities focus on current data.
- Current data and performance improvement activities focus on historical data.
- Decreasing financial liability and performance improvement activities focus on process improvements.
- Decreasing falls and performance improvement activities focus on process improvements.
The primary distinguishing characteristic of risk management when compared and contrasted to performance improvement is that risk management activities focus on decreasing financial liability and performance improvement activities focus on process improvements.
Risk management focuses on decreasing and eliminating things that are risky and place the healthcare organization in a position of legal liability. Some examples of risk management activities include preventing hazards and adverse events such as patient falls and infant abduction and the legal liabilities associated with these events.
Referrals complement the healthcare teams’ abilities to provide optimal care to the client.
- Referrals simply allow the client to be discharged into the community with the additional care they need.
- Nurses facilitate referrals to only the resources within the facility.
When clients have assessed needs that cannot be fulfilled and met by the registered nurse in collaboration with other members of the nursing care team, the registered nurse should then seek out resources, as well as utilize and employ different internal or external resources such as a physical therapist, a clergy member or a home health care agency in the community and external to the nurse’s healthcare agency.
The Safe & Effective Care Environment: Safety & Infection Control Practice Questions
- The sensitizing dose of penicillin can lead to anaphylaxis.
- The second dose of penicillin can lead to distributive shock.
- You should be aware of the fact that about 10% of the population has an allergy to both penicillin and latex.
- You should be aware of the fact that about 20% of the population has an allergy to both penicillin and latex.
The second dose of penicillin can lead to anaphylactic shock which is a form of distributive shock.
The first exposure to penicillin, referred to as the “sensitizing dose”, sensitizes and prepares the body to respond to a second exposure or dose. It is then the second exposure or dose that leads to anaphylaxis, or anaphylactic shock.
It is estimated that approximately 10% of people have had a reaction to penicillin. Some of these reactions are an allergic response and others are simply a troublesome side effect. There is no scientific data that indicates that 10% or 20% of the population has an allergy to both penicillin and latex.
- A 77 year old female client in a client room that has low glare floors.
- An 87 year old female client in a client room that has low glare floors.
- A 27 year old sedated male client.
- A 37 year old male client with impaired renal perfusion.
The 27 year old sedated male client is at greatest risk for falls.
Some of the risk factors associated with falls are sedating medications, high glare, not low glare, floors and other environmental factors such as clutter and scatter rugs, not low glare floors, a history of prior falls, a fear of falling, incontinence, confusion, sensory deficits, a decreased level of consciousness, impaired reaction time, advancing age, poor muscular strength, balance, coordination, gait and range of motion and some physical disorders, particularly those that affect the musculoskeletal or neurological systems; falls are not associated with poor and impaired renal perfusion.
- The nurse should advise clients in a smoke filled room to open the windows.
- The first thing that the nurse should do when using a fire extinguisher to put out a small fire is to aim the fire extinguisher at the base of the fire.
- Rapidly lift and move a client away from the source of the fire when their slippers are on fire.
- The home health care nurse should advise the client that the best fire extinguisher to have in the home is an ABC fire extinguisher.
The home health care nurse should advise the client that the best fire extinguisher to have in the home is an ABC fire extinguisher because this one fire extinguisher is a combination of a type A fire extinguisher, a type B and a type C, which put out all types of fires including common household solids like wood, household oils like kitchen grease and electrical fires.
The nurse should advise the client GET LOW AND GO if a room fills with smoke. They should not take any time to open window.
The first thing to do when using a fire extinguisher is to pull the pin and then aim it at the base of the fire. Later, you would squeeze the trigger and sweep the spray over and over again over the base of the fire. The acronym PASS is used to remember these sequential steps.
When a person has clothing that has caught on fire, the person should STOP, DROP AND ROLL. Tell the person, to STOP, DROP, and to not run, and as you also cover the person with a blanket to smother the fire.
- A tornado that has touched down on the healthcare facility
- A severe cyclone that has destroyed nearby homes
- A massive train accident that brings victims to your facility
- An act of bioterrorism in a nearby factory
A tornado that has touched down on the healthcare facility is an example of an internal disaster because this tornado has directly affected the healthcare facility. Tornados, cyclones, hurricanes and other severe weather emergencies can be both an internal disaster when they affect the healthcare facility and also an external disaster when they impact on the lives of those living in the community. Hurricane Katrina is a good example of a weather emergency that affected not only healthcare facilities but also members of the community.
- Use a slide board.
- Use a mechanical lift.
- Use a gait belt.
- Notify the client's doctor that the client cannot be safely transferred by you.
The best and safest way to transfer this paralyzed client when you suspect that you will need the help of another for the client’s first transfer out of bed is to use a mechanical lift. It is not necessary or appropriate to notify the doctor.
Mechanical lifts are used mostly for patients who are obese and cannot be safely moved or transferred by two people, and also for patients who are, for one reason or another, not able to provide any help or assistance with their lifts and transfers, such as a person who is paralyzed.
A gait or transfer belt and slide boards are assistive devices that can be used to assist with transfers and lifting however, they are not appropriate for this client as based on your assessment.
- Advise the nurse that the legs must be close together for stability during lifting and transfers.
- Advise the nurse that the legs should be one in front of the other and not spread apart during a transfer.
- Validate the nurse’s competency in terms of the application of body mechanics principles during a transfer.
- Validate the nurse’s competency in terms of the application of ergonomics principles during a transfer.
You should validate the nurse’s competency in terms of the application of body mechanics principles during a transfer because the nurse had spread her legs apart during the transfer to provide a wide base of support, which is a basic principle of body mechanics and not ergonomics.
Simply defined ergonomics addresses correct bodily alignment such as the lumbar curve accommodation in an ergonomically designed chair; and body mechanics is the safe use of the body using the correct posture, bodily alignment, balance and bodily movements to safely bend, carry, lift and move objects and people.
- The client has refrigerated foods labelled with an expiration date.
- You assess that the home is free of scatter rugs that many use to protect the feet against hard floors.
- The client uses the FIFO method for insuring food safety.
- The client assures you that the smoke alarm batteries are replaced annually to insure that they work.
When the client assures the nurse that they replace their smoke alarm batteries annually to insure that they work, the assessing nurse should immediately know that the client is in need of education relating to the fact that smoke alarm batteries should be changed at least twice a year.
The client has demonstrated that they are knowledgeable about food safety and environmental safety because they have expiration dates on refrigerated foods, they use the FIFO method for food safety and they do not use scatter rugs which can lead to falls.
The FIFO rule is F irst I n is F irst O ut. In other words, the first foods in the pantry or refrigerator are the first foods that should be consumed or discarded.
- It is clear?
- It is damaging to the lungs.
- It is damaging to the spleen and the liver.
- It leads to the over production of hemoglobin.
Carbon monoxide is particularly dangerous because it is clear, invisible and odorless. Carbon monoxide poisoning can occur when a person is exposed to an excessive amount of this odorless and colorless gas; it severely impairs the body to absorb life sustaining oxygen which is the result of this deadly gas and not damage to the lungs. This oxygen absorption deficit can lead to serious tissue damage and death. For these reasons, home carbon monoxide alarms are recommended.
These dangers are associated with deoxygenation and not splenic or hepatic damage or the over production of hemoglobin.
- Sentinel event.
- System variance.
- Adverse effect.
- Provider variance.
The lack of necessary supplies and equipment to adequately and safely care for patients is an example of a system variance.
A variance is defined as a deviation that leads to a quality defect or problem. Variances can be classified as a practitioner variance, a system/institutional variance, a patient variance, a random variance and a specific variance.
A sentinel event is defined as is an event or occurrence, incident or accident that has led to or may possibly lead to client harm. Adverse effects are serious and unanticipated responses to interventions and treatments, including things like medications.
- Notify the doctor.
- Render care.
- Assess the cleint.
- Notify the nurse manager.
The first thing that you should do immediately after a client accident is to assess the client and the second thing you should do is render care after this assessment and not before it.
Lastly, notifications to the doctor and the nurse manager are only done after the client is assessed and emergency care, if any, is rendered.
- Counsel the staff about their need to stop wasting the resources of this department.
- Check the equipment yourself to determine the accuracy of this equipment department.
- Ignore it because everyone can make an innocent mistake.
- Plan an educational activity about determining what equipment to send for repairs.
You should plan an educational activity about determining what equipment should and should not be sent for repairs. This data suggests that the staff members need education and training about the proper functioning of equipment used on the nursing care unit.
Counseling the staff about their need to stop wasting the resources of this department is placing blame and this blame may prevent future valid returns of equipment.
You should not check the equipment yourself to determine the accuracy of this equipment department because they are the experts, not you, with these matters.
You should also not ignore it because everyone can make an innocent mistake. The issue has to be addressed and corrected.
- Education and training on all pieces of equipment
- Pilot testing new equipment
- Reading all the manufacturer’s instructions
- Researching the equipment before recommending its purchase
Education and training on all pieces of equipment is an essential component for insuring that medical equipment is being used safely and properly by those who you supervise. Other essential components include validated and documented competency to use any and all pieces of equipment by a person qualified to do so, preventive maintenance and the prompt removal of all unsafe equipment from service.
Pilot testing new equipment, researching the equipment before recommending its purchase, and reading the entire manufacturer’s instructions are things done prior to the purchase of the equipment and these things do not impact on the safety of the piece of medical equipment.
- A possible vulnerability of the facility’s information technology to hacking
- The assisted suicide of a client in your facility by the spouse of the client
- Vulnerability to computer hacking
- Potential information theft
The assisted suicide of a client in your facility by the spouse of the client is a security concern that is also a sentinel event that must be reported.
A possible vulnerability of the facility’s information technology to hacking, vulnerability to computer hacking and potential information theft is security concerns but they are not sentinel events that must be reported.
- Training all nurses to serve as a part of a security response team
- Training all clerical staff to be a part of a security response team
- The restriction of visitors in a special care area
- Bar coded client identification bands to insure proper identification
The restriction of visitors in a special care area is an effective security plan that you may want to consider for implementation within your facility.
Some of the other security measures that you may want to consider include security alert systems to alert staff to a security breach such as security breach of the newborn nursery, the use of visitor identification badges or stickers that identify people who are authorized to be in a facility, closed circuit monitoring and alarm systems in high risk areas such as the emergency care area, automatically locking security doors, and electronic wristbands for the newborn and the mother to prevent infant abductions.
Special assignments and training for a group of people so that this specially trained group can act when a security breach occurs is also a good idea but it is not necessary to train all nurses or clerical staff; it is sufficient to train a limited group of people, provided an ample number of these team members are assigned and available on all tours of duty around the clock, including on holidays.
- Sterile items ONLY are placed on the sterile field.
- The nurse must keep the sterile field below waist level.
- Coughing or sneezing over the sterile field contaminates the sterile field.
- The nurse must maintain a 1/2 inch border around the sterile field that is not sterile.
- Moisture and wetness contaminate the sterile field.
- Sterile masks are used by staff and the client when a sterile field is being set up and/or maintained
Correct Response: A, C, E
Sterile items ONLY are placed on the sterile field; coughing or sneezing over the sterile field contaminates the sterile field; and all moisture and wetness contaminate the sterile field.
Some of the other principles that are applied to setting up and maintaining a sterile field include keeping the sterile field above the waist level and preventing coughing or sneezing by professional staff and the client during the set up and during the maintenance of the sterile field. If there is a danger that anyone may cough or sneeze over the field, the professional staff and/or the client should don a mask to prevent contamination. Lastly, a one inch border, not a ½ border that is not sterile is maintained around the perimeter of the sterile field.
- A physical restraint: A physical restraint is a manufactured device that is used, when necessary, to prevent falls.
- A physical restraint: A physical restraint is any mechanical device, material, or equipment attached to or adjacent to the resident’s body that the individual cannot remove easily which restricts freedom of movement or normal access to one’s body.
- A chemical restraint: A chemical restraint is a drug used for sedation to prevent falls.
- A chemical restraint: A chemical restraint is a drug used for discipline or convenience and not required to treat medical symptoms.
A chemical restraint: A chemical restraint is a drug used for discipline or convenience and not required to treat medical symptoms, according to the Centers for Medicare and Medicaid Services.
The most complete and accurate definition of a physical restraint is any manual method or physical or mechanical device, material, or equipment attached to or adjacent to the resident’s body that the individual cannot remove easily which restricts freedom of movement or normal access to one’s body and is NOT a safety devices that is routinely used for certain procedures, according to the Centers for Medicare and Medicaid Services.
- Informed consent for the restraint
- The reason for the restraint
- The type of restraint to be used
- Client behaviors that necessitated the restraints
The minimal components of orders for restraint include the reason for and rationale for the use of the restraint, the type of restraint to be used, how long the restraint can be used, the client behaviors that necessitated the use of the restraints, and any special instructions beyond and above those required by the facility’s policies and procedures.
Informed consent is not necessary for the initiation or the use of restraints
- The vascular phase
- The prodromal phase
- The incubation phase
- The initial injury
- The exudate phase
- The convalescence phase
The stages of the inflammatory process in correct sequential order are:
- The initial tissue injury which can result from an infection or a traumatic cause
- The vascular response. The release of histamine, prostaglandins and kinins. These substances lead to vasodilation which increases the necessary blood supply to the injured tissue and the area surrounding
- The exudate response. The release of leukocytes, including macrophages and neutrophils, to the injured area to combat the infection.
The signs of infection such as the incubation, prodromal and convalescence stages, in the correct sequential order are:
- The incubation period
- The illness stage
- The convalescence stage
Health Promotion & Maintenance Practice Questions
- The infant had doubled their birth weight at twelve months.
- The infant had tripled their birth weight at twelve months.
- The mother reports that the infant is drinking 60 mLs per kilogram of its body weight.
- The infant had grown ¼ inch since last month.
The normal assessment data for the infant at 12 months of age is that the infant has doubled their birth weight at 12 months of age.
The mother’s reports that the infant is drinking 60 mLs per kilogram of its body weight and the fact that the infant had grown ¼ inch since last month are not normal assessment data. Infants are fed breast milk or formula every two to four hours with a total daily intake of 80 to 100 mLs per kilogram of body weight.
As the neonate grows, they gain five to seven ounces during the first six months and then they double their birth weight during the first year; the head circumference increases a half inch each month for six months and then two tenths of an inch until the infant is one year of age. Similarly, the height or length of the newborn increases an inch a month for the first 6 months and then 1/2 inch a month until the infant is 1 year of age.
- The Programmed Longevity Theory
- The Immunological Theory of Aging
- The Endocrine Theory
- The Rate of Living Theory
The theory of aging that supports your belief that strict infection control prevention measures are necessary is the Immunological Theory of Aging. The Immunological Theory of Aging states that aging leads to the decline of the person’s defensive immune system and the decreased ability of the antibodies to protect us against infection.
The Programmed Longevity Theory of aging states that genetic instability and changes occur such as some genes turning on and off lead to the aging process; the Endocrine Theory of aging states that aging results from hormonal changes and the biological clock’s ticking; and Rate of Living Theory states that one’s longevity is the result of one’s rate of oxygen basal metabolism.
Other theories of aging are:
- Wear and Tear Theory: This theory describes aging as a function of the simple wearing out of the tissues and cells as one ages.
- Cross Linking Theory: This theory of aging explains that aging results for cell damage and disease from cross linked proteins in the body.
- Free Radicals Theory: This theory is based on the belief that free radicals in the body lead to cellular damage and the eventual cessation of organ functioning.
- Somatic DNA Damage Theory: Somatic DNA Damage theory is based on the belief that aging and death eventually occur because DNA damage, as continuously occurs in the human cells, continues to the point where they can no longer be repaired and replaced and, as a result, they accumulate in the body.
- Increased creatinine clearance.
- Impaired immune system.
- Decreased hepatic metabolism.
- Increased bodily fat.
The elderly population is at risk for more side effects, adverse drug reactions, and toxicity and over dosages of medications because the elderly have a decrease in terms of their hepatic metabolism secondary to the hepatic functioning changes of the elderly secondary to a decreased hepatic blood flow and functioning.
The elderly have decreased rather than increased creatinine clearance; the immune system is also decreased in terms of its functioning, however, this change impacts on the elderly’s ability to resist infection rather than impacting a medication’s side effects, adverse drug reactions, toxicity and over dosages; and, lastly, a decrease in terms of bodily fat, rather than an increase in terms of bodily fat impacts on medications. The distribution of drugs is impaired by decreases in the amount of body water, body fat and serum albumin; drug absorption is decreased with the aged patient’s increases in gastric acid pH and decreases in the surface area of the small intestine which absorbs medications and food nutrients.
The expected date of delivery is calculated using Nagle’s rule which is:
The first day of last menstrual period – 3 months + 7 days = the estimated date of delivery
For example, when the first day of the last menstrual period is 10/20/2016 you would:
- Subtract three months from 10/20/2016 and then you get 7/20/2016 and then
- Add seven days to 7/20/2016 and then get 7/27/2016, after which you would
- Add one year to 7/27/2016 to get the estimated date of delivery for7/27 of the following year which is 7/27/2017.
- You should explain that fetal lie is where the fetus’ presenting part is within the birth canal during labor, among other information about the other assessments.
- You should explain that fetal presentation is the relationship of the fetus’s spine to the mother’s spine, among other information about the other assessments.
- You should explain that fetal attitude is the relationship of the fetus’ presenting part to the anterior, posterior, right or left side of the mother’s pelvis, among other information about the other assessments.
- You should explain that fetal station is the level of the fetus’ presenting part in relationship to the mother’s ischial spines, among other information about the other assessments.
You should explain that fetal station is the level of the fetus’ presenting part in relationship to the mother’s ischial spines. Fetal station is measured in terms of the number of centimeters above or below the mother’s ischial spines. Fetal station is -1 to -5 when the fetus is from 1 to 5 centimeters above the ischial spines and it is from +1 to +5 when the fetus is from 1 to 5 centimeters below the level of the maternal ischial spines.
Fetal lie is defined as the relationship of the fetus’s spine to the mother’s spine. Fetal lie can a longitudinal, transverse or oblique life. Longitudinal lie, the most common and normal lie, occurs when the fetus’ spine is aligned with the mother’s spine in an up and down manner; a transverse lie occurs when the fetus’ spine is at a right ninety degree angle with the maternal spine; and, lastly, an oblique lie occurs when the fetus’ spine is diagonal to the mother’s spine.
Fetal presentation is defined by where the fetus’ presenting part is within the birth canal during labor. The possible fetal presentations are the cephalic presentation, the cephalic vertex presentation, the cephalic sinciput presentation, the cephalic face presentation, the cephalic brow presentation, the breech presentation, the complete breech presentation, the frank breech presentation, the shoulder breech presentation, and the footling presentation.
Fetal attitude is the positioning of the fetus’s body parts in relationship to each other. The normal attitude is general flexion in the “fetal position”. All attitudes, other than the normal attitude, can lead to a more intense and prolonged labor.
Fetal position is the relationship of the fetus’ presenting part to the anterior, posterior, right or left side of the mother’s pelvis.
- You should apply the principles of initiative when caring for preschool children.
- You should apply the principles of sensorimotor thought when caring for preschool children.
- You should apply the principles of intimacy when caring for the adolescent.
- You should apply the principles of concrete operations when caring for the adolescent.
You should apply the principles of initiative when caring for preschool children. The developmental task for preschool children is initiative, according to Eric Erickson.
The other developmental tasks, according to Eric Erickson are:
- Infant: Trust
- Toddler: Autonomy
- School Age Child: Industry
- Adolescent: Identity formation
- Young Adult: Intimacy
- Middle Aged Adult: Generativity
- Older Adults: Ego integrity
In the correct sequential order, Jean Piaget’s levels of cognitive development include:
- Sensorimotor thought: Infancy to About 2 Years of Age
- Preoperational and symbolic functioning: From 2 to 7 Years of Age
- Concrete operations: 7 to 11 Years of Age
- Formal operations: 12 Years of Age
- Childhood immunizations
- Separation anxiety
The expected life transition should you apply into your practice for these pediatric clients as you are caring for pediatric clients of all ages is puberty.
Throughout the life span, there are several significant expected life transitions that require the person to cope and adjust. Some of these expected life transitions include puberty, maternal and paternal attachments and bonding to the neonate, pregnancy, care of the newborn, parenting, and retirement.
Although young children will experience separation anxiety and they will also be maintained on an immunization schedule, these are not expected life changes.
- The Biophysical Dimension
- The Psychological and Emotional Dimension
- The Spiritual Dimension
- The Health Systems Dimension
The Dimensions Model of Health includes six dimensions that impact on the client, including the community. The Spiritual Dimension is not one of these six dimensions.
These dimensions are the:
- Biophysical Dimension
- Psychological and Emotional Dimension
- Health Systems Dimension
- Behavioral Dimension
- Socio-Cultural Dimension
- Physical Environment Dimension
- Mediterranean ethnicity for cystic fibrosis.
- African American ethnicity for Tay Sachs disease.
- British Isles ethnicity for psychiatric mental health disorders.
- Saudi Arabian ethnicity for sickle cell anemia.
You would identify a client who is of Saudi Arabian ethnicity for sickle cell anemia. Other ethnicities at greatest risk for sickle cell anemia include those who are African, Latin Americans, Southern Europeans and some clients from some Mediterranean nations.
Other disorders and diseases and the ethnicities associated with them are listed below
- Thalassemia: Clients with a Mediterranean ethnicity
- Tay Sachs Disease: Ashkenazi Jewish people
- Cystic Fibrosis: Clients with a European ethnicity
- Psychiatric Mental Health Disorders: African Americans and Native Americans
- Hypertension: African Americans, Pacific Islanders , Native Americans, Alaskan natives, Hispanic and Caribbean clients
- Diabetes: African Americans, Caribbeans, Native Americans and clients from India, Pakistan and Bangladesh
- Cancer: Caucasians and clients from Scotland and Ireland
- The need for a targeted assessment is based on the application of the nurse’s knowledge of pathophysiology and the presenting symptoms.
- The need for a targeted assessment is based on the application of the nurse’s knowledge of developmental needs and developmental delays.
- Targeted assessment is done on an annual basis for existing clients rather than a complete assessment that is done for new clients.
- Targeted assessments consist of a brief medical history and a complete assessment consists of a complete health history and a complete physical assessment.
The need for a targeted assessment is based on the application of the nurse’s knowledge of pathophysiology and the presenting symptoms. Targeted assessments and screenings are done in addition to routine and recommended screenings when a particular disorder has a genetic pathophysiological component for risk and when a client is presenting with a particular sign or symptom.
For example, a targeted assessments relating to nutritional status may be indicated when an infant or young child is listless and not gaining weight according the established criteria; an adolescent may be target screened for visual acuity when a high school teacher reports that the teen does not seem to be able to read things on the blackboard; and a toddler may be target screened when the parent reports that the child is not responding to their name.
- Genetic predisposition
- Lifestyle choices
- High risk behaviors
- An external locus of control
Life style choices are the risk factors that are most likely able to be corrected. Poor life style choices place a person at risk and they are often considered also risky behaviors.
As discussed before, some risks are preventable and correctable and others are not. For example, genetics, age and gender are NOT modifiable risks, but the risks associated with life style choices are modifiable, correctable and able to be eliminated when the person changes their behavior in reference to these risky behaviors.
Some risky life style choices include:
- Excessive sun exposure
- The lack of regular exercise
- A poor diet
- Cigarette smoking and the use of other tobacco products
- Alcohol use
- Illicit drug use
- Unprotected sex
- Avocational and hobby choices such as rock climbing
- Inadequate sleep and rest
Genetic predisposition is an innate and not correctable risk factor and an external locus of control can lead to poor life style choices, however, this is not the most likely correctable risk factor.
- A transdermal contraceptive patch
- A diaphragm
- A vaginal contraceptive ring
You would not recommend any of the above methods of contraception for this family.
You would not recommend the use of a transdermal contraceptive patch or a vaginal contraceptive ring for the couple because both of these contraceptive methods are contraindicated when the woman has a history of deep vein thrombosis and cigarette smoking; and you would also not recommend a diaphragm because the compliance of this couple cannot trusted because the couple has a history of the lack of adherence to medical regimens.
- Information about the lack of scientific evidence regarding the effectiveness of all herbs.
- Data to support the fact that magnets can be effective in terms of fibromyalgia pain, and as such, may be a good choice for this client.
- Research that suggests that prayer is an effective alternative method to relieve pain and stress that can be helpful to this client.
- Information that contraindicates the use of biofeedback because this alternative, complementary health practice can interfere with the client’s pacemaker functioning.
Scientific data now indicates that prayer is effective for the relief of stress, anxiety and pain, and as such, may be helpful to this client.
Some herbs, minerals and supplements are scientifically deemed as safe and effective and others are not scientifically effective and they can also lead to harm; at the current time, the National Institutes of Health (NIH) states that magnets are not scientifically effective and they are also not considered safe for clients with a pacemaker or insulin pump because these internally implanted devices can be adversely affected by the magnetic force of the magnet; and, lastly, biofeedback does not interfere with the client’s pacemaker functioning.
- A social worker
- A physical therapist
- An occupational therapist
- A speech therapist
The healthcare professional would you most likely refer this family to in order to address this deficit in terms of their instrumental activities of daily living (ADLs) is a social worker.
The activities of daily living are differentiated in terms of the basic activities of daily living and the instrumental activities of daily living. Examples of basic activities of daily living include things like bathing, mobility, ambulation, toileting, personal care and hygiene, grooming, dressing, and eating. Deficits in terms of the basic activities of daily living are best addressed by a physical and/or occupational therapist.
The instrumental activities of daily living are more advanced than the basic activities of daily living. The instrumental activities of daily living include things like grocery shopping, housework, meal preparation, the communication with others using something like a telephone, and having transportation. Deficits in terms of the instrumental activities of daily living are best addressed by a social worker. For example, the social worker may assist the client in terms of their transportation and they can also teach the client about how to grocery shop, for example.
- Olfactory Cranial Nerve: The sensory nerve that transmits the sense of smell to the olfactory foramina of the nose
- Optic Cranial Nerve: This sensory nerve transmits the sense of vision from the retina to the brain.
- Oculomotor Cranial Nerve: This motor and sensory nerve controls eye movements and visual acuity.
- Trochlear Cranial Nerve: This motor nerve innervates eye ball movement and the superior oblique muscle of the eyes.
- Abducens Cranial Nerve: This motor nerve innervates and controls the abduction of the eye using the lateral rectus muscle.
- Facial Cranial Nerve: This motor nerve controls facial movements, some salivary glands and gustatory sensations from the anterior part of the tongue.
- Glossopharyngeal Cranial Nerve: This sensory nerve This nerve gives us the sense of taste from the posterior tongue, and it also innervates the parotid glands
Correct Response: A,B,D,E
The olfactory cranial nerve is a sensory nerve that transmits the sense of smell to the olfactory foramina of the nose; the optic cranial nerve is also a sensory nerve and it transmits the sense of vision from the retina to the brain.
The trochlear cranial nerve is a motor nerve that innervates eye ball movement and the superior oblique muscle of the eyes; and the abducens cranial nerve is a motor nerve that innervates and controls the abduction of the eye using the lateral rectus muscle.
The oculomotor cranial nerve is a motor nerve controls eye movements, the sphincter of the pupils and the ciliary body muscles; it has no sensory function. The facial cranial nerve is a motor and sensory nerve which controls facial movements, some salivary glands and gustatory sensations from the anterior part of the tongue. And, lastly, the glossopharyngeal cranial nerve is both a motor and sensory nerve that gives us the sense of taste from the posterior tongue, and it also innervates the parotid glands.
- The Taylor test
- The Rinne test
- The Babinski test
- The APGAR test
The sense of hearing is assessed using the Rinne test and the Weber test and a tuning fork.
A Taylor hammer, not a Taylor test, is used to check reflexes like the biceps and triceps reflexes; the Babinski sign occurs when the foot goes into dorsiflexion and the great toe curls up; this sign is an abnormal response to this stimulation and it can indicate the presence of deep vein thrombosis. And lastly, the APGAR test is used to assess the neonate immediately after birth in terms of the infant’s appearance, grimace and reflexes, appearance in terms of skin color, and respiratory rate and effort.
- Light palpation
- Deep palpation
Deep palpation is cautiously done after light palpation when necessary because the client’s responses to deep palpation may include their tightening of the abdominal muscles, for example, which will make the light palpation less effective for this assessment, particularly if an area of pain or tenderness has been palpated.
Inspection is typically the first step and percussion of the abdomen should be done prior to any palpation, particularly deep palpation.
The five types of sounds that are elicited during percussion are flatness, resonance, hyperresonance, tympany and dullness. Dullness is heard when percussion is done over a solid organ like the liver and spleen.
Flatness is normally assessed over muscles and bones; resonance is a hollow sound that is heard, for example, over the air filled lungs; and hyperresonance, which is a booming sound that is heard over abnormal lung tissue, as occurs among clients with chronic obstructive pulmonary disease (COPD); and, lastly, tympany is heard over the stomach with air as a drum like sound.
- A complete medical history, a general survey and a complete physical assessment.
- A complete medical history, a general survey and a focused physical assessment.
- A client interview, a significant other interview, a general survey and a complete physical assessment.
- A client interview, a significant other interview, a general survey and a focused physical assessment.
A comprehensive health assessment includes a complete medical history, a general survey and a complete physical assessment.
Although a complete medical history is done using a client interview and a significant other interview for much data, it is the health history and not the interview that is part of the comprehensive health assessment. A focused assessment is done as based on some pathology, sign or symptom and it is not considered a part of a comprehensive health assessment.
- Tympany: A hollow sound
- Dullness: A thud like sound
- Dullness: A hollow sound
- Resonance: A booming sound
Dullness is a thud like sound and not a hollow sound. Tympany is a drum like sound; and resonance is a hollow sound.
Psychosocial Integrity Practice Questions
- A couple which consists of a husband and wife both of whom are affected with Alzheimer’s disease
- A poverty stricken couple without any healthcare resources in the community
- A pregnant woman and a husband who was physically abused as a young child
- A wealthy couple with feelings that they are immune from punishment and above the law
A pregnant woman and a husband who was physically abused as a young child is the couple is at most risk for domestic violence because pregnancy and a personal prior history of abuse are two commonly occurring risk factors among abused woman and male abusers, respectively.
Current research indicates that abuse and neglect affect all people of all ages and of all socioeconomic classes including the wealthy as well as the poverty stricken.
Other patient populations at risk of abuse and neglect include female gender, infants, children, the cognitively impaired, the developmentally challenged, the elderly and those with physical or mental disabilities; some of the other traits and characteristics associated with abusers include substance related use and abuse, a psychiatric mental health disorder, poor parenting skills, poor anger management skills, poor self-esteem, poor coping skills, poor impulse control, immaturity, and the presence of a current crisis.
- Restrain the client
- Place the client in seclusion
- Get an order for a sedating medication
- Establish trust with the client.
The first thing that you should do to prevent violence towards others is to establish trust with the client. The first step in the nurse-client relationship is to establish trust in this therapeutic relationship. Without trust future collaboration, interventions and client outcomes cannot be accomplished to facilitate appropriate and safe behaviors.
Restraints and seclusion are not indicated until others are in imminent danger because of this client’s current violent behaviors and not a history of it. Lastly, sedating medications to prevent violence are also not the first things that are done.
- Psychological dependence secondary to amphetamine use
- Substance abuse secondary to amphetamine use
- Addiction secondary to amphetamine use
- Physical dependence secondary to amphetamine use
The appropriate nursing diagnosis for this client is “Psychological dependence secondary to amphetamine use”. Psychological dependence is defined as the person’s need to continue the use of the substance to avoid any unpleasant feelings and experiences that can occur when the substance is not taken. Amphetamines and hallucinogenic drugs like LSD are often associated with psychological dependence.
Substance abuse, simply defined, is one’s overindulgence of an addictive substance which can be alcohol, prescription drugs and/or illicit, illegal drugs. Substance abuse does not include prescribed medications, such as narcotic pain medications, that are being used for medical reasons; however, these same medications when used after there is no longer a medical need to use them is considered substance abuse.
Addiction is defined as the unending and constant need for the person to have the chosen substance even when the use of the substance causes the client to have serious physical, psychological, social and/or economic consequences and harm including a loss of control over the substance abuse and use. Contrary to popular opinion, addiction can occur with and without physical dependence.
Physical dependence occurs when the cessation of a drug causes adverse physical effects; these ill effects are typically greater and more intense when the cessation of the drug is rapid and abrupt. Some of the drugs that are most often associated with physical dependence include cocaine, opioid drugs, alcohol and benzodiazepines. As previously stated, physical dependence does not necessarily indicate addiction; addiction can be present with or without any physical dependency.
- Orem’s Self Care Model
- Nagi's Model
- A cognitive model of disability
- A biomedical model of disability
Nagi’s Model of disability model describes disabilities and its limitations are the result of a discrepancy between the client’s abilities and the limitations of the physical and social environment within which the client lives.
Although clients with disabilities should be assessed and have interventions related to their self care abilities, Dorothea Orem’s Self Care Model is not a model of disability. This model describes self care needs and abilities as wholly compensatory, partly compensatory and supportive educative.
Cognitive models of disability focus on the importance of affected client’s ability to remain as independent as possible and ways that the empowered client can exercise their own self-determination, confidence, self efficacy, and control.
Lastly, biomedical models address pathology, impairments and the manifestations of impairments that can be cured or lead to death.
The characteristics of the stages or phases of crisis, in the correct sequential order, are:
- Level 1 Crisis Signs and Symptoms: Patients experiencing a level one crisis typically experience anxiety and they also typically begin to use one or more psychological ego defense mechanisms.
- Level 2 Crisis Signs and Symptoms: Patients experiencing a level two crisis most likely exhibit some loss of their ability to function. They may also try to experiment with alternative methods of coping in order to deal with the crisis that is not being effectively coped with using one’s currently used coping mechanisms.
- Level 3 Crisis Signs and Symptoms: Patients experiencing a level three crisis show the signs and symptoms of the General Adaptation Syndrome which is characterized with fight, flight and panic as discussed above under the section entitled “Coping Mechanisms: Introduction”.
- Level 4 Crisis Signs and Symptoms: Clients experiencing a level four crisis exhibit severe signs and symptoms such as being totally detached and removed from others, feeling overwhelmed, becoming disoriented, and even with thoughts of violence toward self and others.
- Displacement
- Sublimation
- Dissociation
- Reaction formation
Dissociation is the psychological ego defense mechanism occurs when the client detaches and dissociates with person or time to avoid the stress until they are ready to cope with it.
Displacement transforms the target of one’s anger and hostility from one person to another person or object. Displacement allows the person to ventilate and act out on their anger in a less harmful and a more socially acceptable manner.
A client uses the ego defense mechanism of sublimation when they transform and replace unacceptable urges and feelings into a socially acceptable urge or feeling.
A client is using reaction formation when the client acts and behaves in a manner that is completely the polar opposite of their true feelings.
- Jean Watson's
- Martha Rogers'
- Nagi's theory
- Madeleine Leininger’s theory
The theoretical framework that you would recommend that this committee should consider when addressing mutiethnicity and the culturally diverse nature of this facility for this philosophy is Madeleine Leininger’s theory.
Madeleine Leininger’s theory of Transcultural Nursing and her book “Culture Care Diversity and Universality: A Theory of Nursing” “searches for comprehensive and holistic care data relying on social structure, worldview, and multiple factors in a culture in order to get a holistic knowledge base about care” (Leininger, 2006, p. 219)
Jean Watson’s Jean Watson developed the Human Caring Theory which states that caring is the essence of nursing. Watson's theory has the four major concepts of health, nursing, society/environment and human being. Caring consists of the following 10 nursing interventions that demonstrate genuine caring.
Martha Rogers’ theory is the Science of Unitary Human Beings which is based on general systems theory without any focus on multiethnicity and cultural diversity; and lastly, Nagi’s Model of disability model describes disabilities and its limitations are the result of a discrepancy between the client’s abilities and the limitations of the physical and social environment within which the client lives.
- The client will accept impending death
- Guilt related to past transgressions
- Spiritual distress related to guilt
- Pain related to end of life symptoms
“The client will accept impending death” is the client goal would be the most likely appropriate and expected for the vast majority of these clients. In fact, one of the primary goals of hospice and palliative care is to facilitate the client’s and family member’s acceptance.
Other goals are the freedom for guilt, spiritual distress and pain at the end of life; therefore, these diagnoses are not expected.
- The client will be free of constipation
- The client will remain free of pain and distress
- The administration of an antiemetic to prevent vomiting and further dehydration
- The administration of an enema to correct the constipation
Based on this client’s signs and symptoms and the fact that the client is expected to die in a day or two, the appropriate client outcome for this client is that the client will remain free of pain and distress.
“The client will be free of constipation” requires interventions such as an enema which are not indicated when death is imminent unless, of course, the client is adversely affected with pain and discomfort as the result of it which is not the case with this client. Additionally, the administration of an antiemetic to prevent vomiting is not indicated because there is no evidence in this question that the client is actually vomiting.
- “You should try to come to a few sessions at least because they may be very informative to you”.
- “You are probably correct. This really is not your problem”.
- “Despite the fact that it is your grandson’s drug addiction, situations such as this affect all members of the family including grandparents who live in the home.”
- "You should attend because the doctor has ordered family therapy for you as extended family members”.
You should respond to the grandparents’ statement with “Despite the fact that it is your grandson’s drug addiction, situations such as this affect all members of the family including grandparents who live in the home”.
After this statement, you should also educate the grandparents about the fact that group and family therapy is often indicated when the family unit is affected with stressors and dysfunction because family members may not fully understand the need for the entire family unit to participate when only one member of the family is adversely affected with a stressor and poor coping and that all family members are affected when only one member of the family unit is adversely affected.
You would NOT state “You should try to come to a few sessions at least because they may be very informative to you” because these sessions are therapeutic and not educational; you would not state “You are probably correct. This really is not your problem” because this statement is not true; and you should also not state “You should attend because the doctor has ordered family therapy for you as extended family members” because this is not the real reason why attending these sessions is needed.
- Engel's theory
- Kubler Ross' theory
- Lewin's theory
- Warden's theory
The theory of grief and loss would you most likely integrate into your practice as you perform this role is Warden’s Four Tasks of Mourning. This theory has four tasks that people go through after the loss of a loved one. These tasks are accepting the loss, coping with the loss, altering, modifying and changing the environment to cope with and accommodate for the absence of the lost person, and, finally, resuming one’s life while still having a healthy connection with the loved one.
Engel’s Stages of Grieving include stages both prior to and after a loss and these stages are:
- Shock and disbelief
- Developing awareness
- Restitution
- Resolving the loss
- Idealization
Kubler Ross’s Stages of Grieving occur prior to the death and these stages include:
Lastly, Lewin developed theories of change, leadership and conflict and NOT a theory related to grief after the loss of a loved one.
- The concern related to the client’s cultural reluctance to report psychological symptoms because of some possible culturally based stigma associated with psychiatric mental health disorders
- Concerns revolving around the lack of financial and health insurance resources to pay for psychological care
- Concerns related to the compliance with psychological treatment regimens because of the client’s lack of social support systems
- The concern related to the culturally based client apathy about nursing care and nursing assessments
The concern related to the client’s cultural reluctance to report psychological symptoms because of some possible culturally based stigma associated with psychiatric mental health disorders which is a barrier to assessment because the client fears being stigmatized and rejected when divulging psychological data including anxiety and other symptoms.
The lack of financial and health insurance resources to pay for psychological care, the lack of social support systems, and the client’s apathy are barriers to psychological care but these factors are not a barrier to a psychological assessment and these factors are not cultural, but instead social and psychological.
- Cognitive psychotherapy
- Behavioral psychotherapy
- Cognitive behavioral psychotherapy
- Psychoanalysis
Behavioral psychotherapy is particularly useful among clients who are adversely affected with phobias, substance related disorders, and other addictive disorders. Some of the techniques that are used with behavioral therapy include operant conditioning as put forth by Skinner, aversion therapy, desensitization therapy, modeling and complementary and alternative stress management techniques.
Cognitive psychotherapy is most often used to treat clients, including groups of clients, with depression, eating disorders, anxiety, and anxiety disorders to facilitate the altering of the clients’ attitudes and perspectives relating to stressors.
Cognitive behavioral psychotherapy, which is a combination of cognitive psychotherapy and behavioral psychotherapy and also referred to as dialectical behavioral therapy is most often used for clients affected with a personality disorder and those at risk for injury and harm to self and/or others.
Psychoanalysis, in contrast to cognitive behavioral therapy and other individual and group therapies, dives into the client’s subconscious and it often focuses on the past as well as the client’s current issues. This therapy is not conducted by registered nurses but, instead, by experienced psychotherapists.
The client religion that is the most pertinent to the role of the admissions coordinator of hospital who assigns the rooms and beds of clients who will be admitted is the Islam religion which requires that the followers face Mecca for daily prayer, therefore, Islam clients should be placed in a room that faces the holy city of Mecca.
Although most religions impact on the care of the client, only Islam is pertinent to the admissions coordinator. Other religions practices and their impact on health care are shown below:
- Christians: End of life rituals like the Sacrament of the Sick, baptisms for newborns, fasting, and the Eucharist.
- Judaism: Religious based circumcisions, a kosher diet which separates dairy foods from meat based foods, and death rituals called a Shiva.
- Hinduism: Many followers are vegetarian; personal hygiene is paramount and they also have death rituals without the prolongation of life.
- Mormonism: Baptism for the newborn, last rites at the time of death, communion, and burials of the dead. Additionally, the Mormon religion prohibits alcohol, tobacco, and caffeine.
- Jehovah’s Witnesses: Prohibitions against blood transfusions, foods containing blood, homosexuality, sex before marriage, abortion, suicide, gambling, alcoholic beverages, tobacco and illicit drugs.
- Psychotic symptoms related to sensory overload
- Psychotic symptoms related to a previously undiagnosed psychosis
- Visual disturbances related to dementia
- Visual disturbances related to delirium
“Visual disturbances related to delirium” is the most appropriate nursing diagnosis for this client, as based on their signs, symptoms, past history and current medical status.
Delirium is characterized with a sudden and abrupt onset of episodic and intermittent periods of time vacillating between periods of impaired cognition and periods of mental clarity. Visual hallucinations are a sign of delirium and delirium can result from a number of different causes including dehydration and anticholinergic medications.
The signs and symptoms of sensory overload do not include visual hallucinations and a sudden and abrupt onset of episodic and intermittent periods of time vacillating between periods of impaired cognition and periods of mental clarity. Instead, the signs and symptoms of sensory overload include anxiety, restlessness, sleep deprivation, fatigue, poor problem solving and decision making skills, poor performance, and muscular tension.
There is no evidence in this question that the client has psychotic symptoms related to a previously undiagnosed psychosis; all the evidence substantiates the suspicion that the client is affected with delirium.
Lastly, dementia has a gradual and progressive onset rather than an abrupt and sudden onset.
- Collect baseline blood pressure readings prior to the beginning of this educational series and then collect and compare blood pressure data during the series and after the series is completed.
- Collect baseline blood pressure readings prior to the beginning of this educational series and then collect and compare blood pressure data after the series is completed.
- Ask the clients how often they use the stress management techniques that they have learned during this educational series.
- Use a questionnaire at the end of the series that asks the participants how they liked the class and what they learned during this educational series.
The best way to evaluate the effectiveness of this educational series is to collect baseline blood pressure readings prior to the beginning of this educational series and then collect and compare blood pressure data during the series and after the series is completed. This technique entails evaluating the outcomes of the education in terms of changes in the client and it also includes formative evaluation during the series and summative evaluation at the end of the series.
Collecting baseline blood pressure readings prior to the beginning of this educational series and then collecting and comparing blood pressure data after the series is completed gives us only summative evaluation; it does not provide you with formative evaluation.
Because the primary goal of this series is to lower the blood pressures of clients through the use of stress management techniques, asking the clients how often they use the stress management techniques that they have learned during this educational series and using a questionnaire at the end of the series that asks the participants how they liked the class and what they learned during this educational series does not reflect data and information about the effectiveness of the classes in terms of reducing the blood pressures of hypertensive clients.
Tai Chi is a type of a mind body exercise that deeply focuses on breathing, movement and meditation. Yoga is similar to tai chi in that yoga also employs a combination of breathing, movement and meditation.
Reiki is done for the client when the therapist places their hands on or near the person’s body to promote the client’s energy field and its own natural healing processes. Feng shui is an eastern method of decorating using colors, items and the placement of objects in the environment to promote a harmonious relationship of man and its environment; and lastly Jiu Jitsu is a martial art.
- You should advise the couple to move closer to their children so that they can care for their father.
- You should teach the wife about this progressive disease and the need to promote as much independence as possible.
- You should teach the wife about this progressive disease and the need to do all that she can for the husband to avoid his depression and frustration.
- You should advise the couple to decrease their social activities in order to preserve the husband’s dignity and self-esteem.
You should teach the wife about this progressive disease and the need to promote as much independence as possible. Client’s with Alzheimer’s disease and other disabilities, including physical disabilities, should be coached and encouraged to be as independent as possible.
Moving closer to the children may not be appropriate advice particularly if the children are unable or unwilling to care for their father. Lastly, you should advise the couple to continue their social activities and to only avoid those situations where the necessary compassion and understanding about the client and his condition are absent.
- According to the Global Deterioration Scale, clients in the first stage of Alzheimer’s disease tend to cover up their failing abilities
- According to the Reisberg Scale, clients in the first stage of Alzheimer’s disease tend to cover up their failing abilities
- According to the Global Deterioration Scale, clients in the third stage of Alzheimer’s disease tend to cover up their failing abilities
- According to the Reisberg Scale, clients in the fourth stage of Alzheimer’s disease tend to cover up their failing abilities
According to the Global Deterioration Scale, also referred to as the Reisberg Scale, clients in the third stage of Alzheimer’s disease tend to cover up their failing abilities.
The Global Deterioration Scale stages Alzheimer’s according to seven stages. These stages include
- Stage 1: Cognitive abilities are intact.
- Stage 2: Minimal and hardly noticeable forgetfulness occurs.
- Stage 3: Mild changes in terms of cognition occur. The client may have difficulty in terms of their memory, which at times the client may “cover up” to avoid the detection by others. The signs and symptoms of this stage are similar to those of the Early Stage of Alzheimer’s disease, as discussed immediately above.
- Stage 4: This stage is characterized with increasing confusion about recent events and conversations, mild problems with math and some rather routinized sequential tasks such as cooking. The client may withdraw from others and debate the fact that they are having some cognitive issues.
- Stage 5: Early Dementia occurs. Short and long term memory losses, a lack of orientation to place and time, poor judgment, and some of the client’s self care in terms of the activities of daily living become progressively more problematic. The client may need the assistance and supervision of others to promote the client’s highest possible level of independence in the performance of their basic activities of daily living.
- Stage 6: This stage is referred to a Middle Dementia and moderately severe Alzheimer’s disease. There is almost complete short term and long term memory loss, communication is highly limited and it may only consist of nonverbal behavioral responses, and the client needs complete care to manage their activities of daily living. Sundowner’s syndrome is present and hallucinations as well as agitation may occur.
- Stage 7: This stage is referred to as Late or Severe Dementia and Failure to Thrive. The client is in need of complete care; and immobilization, in addition to the hazards of immobility, may affect the client and the family members at this stage.
- Probing for more information from the client
- Sublimation to determine hidden messages
- Providing privacy so the client is comfortable
- Silence to allow contemplation and thought
- A safe environment of care that is conducive to the prevention of medical errors.
- A client care area that provides personal privacy and the confidentiality of medical information.
- A European method of design and color to promote health and wellness.
- The provision of a therapeutic environment of consistency to promote health.
A therapeutic milieu eliminates as many stressors from the environment as possible. The goal of this environment is to facilitate the client’s coping and recovery without the need to cope with these extraneous and avoidable stressors. Some of the elements of a therapeutic milieu environment include consistency, client rules, limitations and boundaries, and client expectations, including contracts, relating to appropriate behavior.
Physiological Integrity: Basic Care & Comfort Practice Questions
- Psychomotor domain: The client will slightly bend their elbows when holding the hand grips.
- Psychomotor domain: The client will rest their weight on the padded areas on the top of the crutches.
- Cognitive domain: The client will slightly bend their elbows when holding the hand grips.
- Cognitive domain: The nurse will tell the client how often the tips on the crutches must be replaced.
The client goal that is paired with its learning domain that should be included in the patient teaching plan for this client and the parents is “The client will slightly bend their elbows when holding the hand grips” which is part of the psychomotor domain and not the cognitive domain. Lastly, the “nurse will” is an intervention and not a client goal or expected outcome which should be learner, not nurse, oriented.
- An aphasia aid
- A button hook
- Honey thickened liquids
- A word board
The basic activity of daily living assistive device can be useful for the client who is affected with poor fine motor coordination is a button hook that would be used for the dressing activity of daily living.
An aphasia aid and a word board are assistive devices to facilitate communication when the client is affected with a communication deficit such as aphasia; and, lastly honey thickened liquids are indicated for clients with a swallowing disorder and they are not indicated for clients with poor fine motor coordination.
- Place the client in a wheelchair to protect their safety in the clinic.
- Remove the cane from the client to protect their safety.
- Teach the client about the proper length of a cane.
- Have the client use a wheelchair rather than the cane.
You should teach the client about the proper length of a cane. The proper length of the cane should be the length that only permits the client’s elbow to be slightly flexed. Some canes like a wooden cane are not adjustable to the client’s height and others can be adjusted to meet the height needs of the client.
You would not place the client in a wheelchair or ask the client to use a wheelchair and you would also not take the cane, which is their personal property, away from them. You would use this observation as a learning need assessment and, as such, you should teach the client about the proper length of a cane and help them to adjust the height of the cane if the client’s cane is a height adjustable one.
- A cleansing enema
- A retention enema
- A return-flow enema
The most likely intervention for this client, after getting a doctor’s order, is a return flow enema. Return-flow enemas, similar to a carminative enema, are used to relieve flatus and stimulate peristalsis which is frequently a problem after a client has received anesthesia.
Cleansing enemas are used to relieve constipation; and a retention enema is used to administer a medication, to soften stool and to lubricate the rectum so that it is easier and more comfortable for the client to defecate.
Finally, the data in this question does not indicate that the client is constipated and in need of a laxative.
- Both can lead to infection.
- Both are invasive procedures.
- Both are considered sentinel.
- Both are the last resort.
The commonality that is shared in terms of both restraints and urinary catheters is that both are the last, not the first, treatment of choice. Both indwelling urinary catheters and restraints pose risks and complication; therefore, both of these interventions must be prevented with the use of preventive measures.
Indwelling urinary catheters are invasive but restraints are not invasive; indwelling urinary catheters can lead to infection but restraints do not. Lastly, neither are sentinel. A sentinel event is an event or occurrence, incident or accident that has led to or may have possibly led to client harm. Even near misses, that have the potential for harm, are considered sentinel events because they have the potential to cause harm in the future.
- Any solid skin barrier
- A hydrocolloid solid skin barrier
- Hollister’s Flextend
- A skin sealant
You would recommend a skin sealant, including products like Bard’s Protective Barrier and Convatec’s Allkare, which are a fast drying polymer transparent film that can be applied relatively simply with a wipe or a spray. These products are easy to use and less expensive than solid skin barriers, including Hollister’s Flextend and others containing hydrocolloids.
- A prolapsed stoma
- A vitamin B12 deficiency
- Nocturnal enuresis
- GI stone formation
Some of the complications associated with a colostomy include a prolapsed stoma, infection, dehiscence, an ischemic ileostomy, a peristomal hernia, stoma stenosis, stomal retraction, necrosis, mucocutaneous separation, stomal trauma, peristomal skin damage as the result of leakage and parastomal hernias.
A vitamin B12 deficiency, nocturnal enuresis and urinary stone formations are complications associated with urinary diversion and not fecal ostomy diversions.
- Bone demineralization: Turning and positioning every 2 hours
- Urinary stasis: The client will consume 1,000 mL of oral fluids per day
- Muscle atrophy: The client will perform range of motion exercises at least 3 times a day
- Hypercalcemia: Maintaining fluid intake of 1,000 mL per day
“The client will perform range of motion exercises at least 3 times a day” is an appropriate expected outcome of care that the nurse provides to prevent this complication.
Urinary stasis and hypercalcemia, both hazards of immobility, can be prevented when the client will consume 2,000 mL of oral fluids per day. Lastly, calcium loss from the bones can be prevented by weight bearing activity, and not turning and positioning in bed.
- 1 on the scale of 1 to 3
- 2 on the scale of 1 to 5
- 3 on the scale of 0 to 5
- 4 on the scale of 0 to 5
You would document this client’s muscular strength as a 3 on a scale of 0 to 5.
Muscular strength is classified on a scale of zero to five, as below.
- Zero: No muscular contraction
- One: No muscular movement, only a quiver is noted
- Two: Muscular movement but only when assisted with gravity
- Three: Muscular movement against gravity but not against resistance
- Four: Muscular movement against resistance
- Five: Full muscular movement and strength
You would document the size of this wound as 24 cm. After the wound is assessed and measured, the wound dimension is calculated by multiplying the length by the width by the depth of the wound. For example when the length of the sound is 3 cm deep, 2 cm long and 4 cm wide, it is calculated with 3 x 2 x 4 = 24 cm.
- Secondary intention healing
- Tertiary intention healing
- Primary prevention healing
- Secondary prevention healing
Secondary intention healing is the most likely type of wound healing for this client because of the risks associated with the deep infection associated with the ruptured appendix and the peritonitis.
Secondary intention healing, also referred to as healing by second intention, is done for contaminated wounds in order to prevent infections, to prevent the formation of abscesses and to promote healing from the bottom up to the outer surface of the skin so that any potential infection is not closed in at the bottom of the wound. These open wounds are irrigated with a sterile solution and then packed to keep them open and, over time, they will heal on their own. The resulting scar is more obvious than those scars that result from primary intention healing.
Primary intention healing is facilitated with wounds without infection. The wound edges are approximated and closed with a closure technique such as suturing, Steri Strips, and surgical glues.
Tertiary intention healing, also referred to as healing by tertiary intention, is a combination of secondary and primary healing. Tertiary intention healing begins with several days of open wound irrigations and packing, which is secondary healing, followed by the closure of the wound edges with approximation and suturing which is primary healing. Some traumatic wounds are healed with tertiary intention.
Primary, secondary and tertiary prevention strategies are prevention, interventions and restorative or rehabilitation care and not methods of wound healing.
- A barrier film
- An alginate dressing
- Surgical laser debridement
- Autolytic debridement
The treatment of pressure ulcers is complex and it often includes a combination of treatments and therapies. The RYB Color Code of Wounds is sometimes used by nurses to guide the treatment options. RYB stands for the colors of red, yellow and black. The rules of treatment for these three colors are:
- Red: Covering with a dressing such as a hydrocolloid film, turning and positioning the client and avoiding pressure, friction and shearing
- Yellow: Using an alginate dressing
- Black: Debridement, including surgical laser debridement, mechanical debridement, autolytic debridement, enzymatic debridement and sharp instrument debridement, of the area to remove the black necrotic eschar.
- Moritz Schiff’s theory of pain
- The Intensive Theory of Pain
- Melzack and Wall’s theory of pain
- The Specificity Theory of Pain
Melzack and Wall’s Gate Control Theory of pain supports the belief that some of the factors that open this “gate” to pain are low endorphins and anxiety and that some of the factors that close this “gate” to pain are decreased anxiety and fear. The substantia gelatinosa is the “gate” that facilitates or blocks the transmission of pain.
The Specificity Theory of Moritz Schiff described pain as a sensation that was different from all the other senses in that pain had its own specific nervous system pathways from the spinal cord that traveled to the brain; the Intensive Theory of pain is based on the belief that pain is an emotional state, rather than a sensory phenomenon; the Peripheral Pattern Theory of pain of Sinclair and Weddell describes pain as the result of an intense stimulus applied to the skin; and the Neuromatrix Theory of Pain supports the fact that pain is a dynamic and multidimensional process with physical, behavioral, perceptual, psychological and social responses and one that can only be described by the person who is experiencing it.
- Pain level, the quality of the pain, the region or area of the pain, the severity of the pain, and the pain triggers
- Precipitating factors, the quality of the pain, relief factors, the severity of the pain, and the pain triggers
- Pain level, the quantitative numerical pain score, the region or area of the pain, the severity of the pain, and the pain triggers
- Precipitating factors, the quality of the pain, the region or area of the pain, the severity of the pain, and the pain triggers
Precipitating factors, the quality of the pain, the region or area of the pain, the severity of the pain, and the pain triggers are the PQRSTs of the PQRST method of pain assessment.
The severity of the pain, which can include a quantitative, numerical pain score from 1 to 10, for example, is the S of the PQRST method of pain assessment.
- Assessment data, biochemical data, clinical data and dietary data
- Ancestral cultural data, biochemical data, clinical data and dietary data
- Anthropometric data, biological data, chemical data and dietary data
- Anthropometric data, biochemical data, clinical data and dietary data
Anthropometric data, biochemical data, clinical data and dietary data are the A, B, C and Ds of a complete and comprehensive nutritional assessment.
The elements of these A, B, C and Ds of nutritional assessment include:
- A: Anthropometric Data: This data includes variables such as height, weight, body mass index and arm measurements such as the mid arm circumference and the triceps skin fold.
- B: Biochemical Data: Laboratory testing data like serum albumin, hemoglobin, urinary creatinine, and serum transferrin.
- C: Clinical Data: The client’s skin condition, level of activity and status of the client’s mucous membranes.
- D: Dietary Data: This data includes the client’s subjective reports of their food and fluid intake over the last 24 hours and the types of foods that are typically eating.
- Constipation: The provision of a high fiber diet
- Urinary pH changes: Encouraging ample oral fluid intake
- Aspiration: Maintaining the client in at least a 30 degree angle
- Aspiration: Maintaining the client in at least a 90 degree angle
Aspiration can be prevented by maintaining the client in at least a 30 degree angle; a 90 degree angle is not only not necessary, this angle places a client at greater risk for the development of a pressure ulcer.
Diarrhea, rather than constipation is a complication of tube feedings; and urinary pH changes are not a commonly occurring complication of tube feedings.
Some of the other complications and preventive measures are:
- Diarrhea: Maintaining a slow rate of infusion whenever possible, changing the ordered rate and formula when necessary
- Abdominal pain: Maintaining a slow rate of infusion whenever possible
- Dehydration: Monitor the client for any signs and symptoms of dehydration, measure intake and output and notify the doctor of any abnormalities
- Nausea and Vomiting: Slowing the rate down, changing the formula and antiemetic medications to stop the vomiting and to prevent any aspiration
- Tube Dislodgment: Secure and monitor the tube
- Locus of control
- Bodily surface area
- Diaphoresis
There are a wide variety of different factors that influence and impact on our clients’ hygiene habits and routines. For example, cultural practices and beliefs, ethnical factors, religious practices and beliefs, the client’s level of growth and development.
Although the locus of control, bodily surface area and diaphoresis in addition to other factors such as economic constraints, the client’s level of energy, the client’s level of cognition, and environmental factors can impact on hygiene, these are not factors that impact on the client’s hygiene and hygiene practices; they do not typically impact on the lifelong developed hygiene and hygiene practices.
- The neonate: 10 to 15 hours a day
- The toddler: 11 to 14 hours a day
- The preschool child: 12 to 15 hours a day
- The school age child: Less than 8 hours a day
The age group that is accurately paired with the normal and recommended hours of sleep each day is the toddler should sleep about 11 to 14 hours per day.
The neonate should sleep 14 to 17 hours per day; the preschool child should sleep 10 to 13 hours per day; and the school age child should sleep 9 to 11 hours per day.
Physiological Integrity: Pharmacological & Parenteral Therapies Practice Questions
- Stop the intravenous flow
- Slow down the intravenous flow
- Notify the doctor
Your first priority intervention is to immediately stop the flow of the intravenous antibiotic because it is highly likely that the signs of anaphylaxis have occurred as the result of the client’s adverse effect to this antibiotic.
The next thing that you would do is assess the client to determine their physical status and to provide necessary emergency measures, including CPR, if it is indicated. Later, you would notify the doctor about this adverse reaction.
- Mix a small amount of the medication in a small amount of the intravenous fluid and then examine this mixture for color changes
- Refer to a compatibility chart
- Call the doctor and ask if the medication is compatible with the particular intravenous fluid
- Mix a small amount of the medication in a small amount of the intravenous fluid and then examine this mixture for any precipitates
The best way to determine whether or not a medication is compatible for a particular intravenous fluid is to refer to a compatibility chart.
Although, at times, incompatibility can be evidenced with changes such as those related to color changes and the formation of a cloudy solution or obvious precipitate, at other times incompatibility may not be noticeable. For this reason, nurses must refer to a compatibility or incompatibility chart before they mix medications or medications and solutions.
Lastly, there is no need to call the doctor for compatibilities when you have, and should use, a compatibility chart.
- Prevent polypharmacy
- Conserve financial resources
- Prevent interactions
- Prevent allergies
The medication reconciliation process to insure that the nurse is aware of all medications that the client is taking, some of which may have been ordered by a physician other than the client’s primary care doctor and some of which are over the counter or alternative therapies that the client has added. The complete and current list of medications is then reviewed by the nurse and possible interactions are identified and addressed with the client.
Although this medication reconciliation process can also save costs by eliminating unnecessary medications, particularly when the client is taking multiple medications (polypharmacy), this is not a primary purpose. Lastly, medications that the client is allergic to should never be given, therefore, these medications should not appear during the medication reconciliation process; they should never have been given to or taken by the client.
- The fact that drugs classified as categories C, D and X are contraindicated for women who are pregnant.
- The fact that drugs classified as categories A, B and C are contraindicated for women who are pregnant.
- The fact that drugs classified as categories C, D and E are contraindicated for women who are pregnant.
- The fact that drugs classified as categories C, D and Z are contraindicated for women who are pregnant.
Drugs classified as categories C, D and X are contraindicated for women who are pregnant because of the risks associated with these categories in terms of the developing fetus when these medications cross the placental barrier.
- The nurse must be knowledgeable about the fact that this client has A and B agglutinins and lacks the Rh factor
- The nurse must be knowledgeable about the fact that this client has B and O agglutinins and lacks the Rh factor
- The nurse must be knowledgeable about the fact that this client has B agglutinins and lacks the Rh factor
- The nurse must be knowledgeable about the fact that this client has A agglutinins and lacks the Rh factor
The nurse must be knowledgeable about the fact that this client has A agglutinins and they lack the Rh factor.
Type A blood has B agglutinins; type B blood has A agglutinins, type AB blood has no antibodies, or agglutinins, and type O blood has both A and B agglutinins.
People also have a rhesus, or Rh, factor antigen or the lack of it. Clients with an Rh positive blood, which is the vast majority of people, have Rh positive blood and people without the Rh factor antigen have Rh negative blood.
- Hemolysis: Typing and cross matching the blood and checking for ABO compatibility prior to administration
- Hemolysis: Insuring that the client does not have a prior history of hemolysis in the past
- Febrile reactions: Insuring that the client does not have a prior history of hemolysis in the past
- Febrile reactions: Typing and cross matching the blood and checking for ABO compatibility prior to administration
Hemolysis can be prevented by typing and cross matching the blood and checking for ABO compatibility prior to administration. This incompatibility can occur as the result of a laboratory error in terms of typing and cross matching and a practitioner error in terms of checking the blood and matching it to the client’s blood type.
Febrile reactions are the most commonly occurring reaction to blood and blood products administration. Although a febrile reaction can occur with all blood transfusions, it is most frequently associated with packed red blood cells and this reaction is not accompanied with hemolysis nor is it associated with its occurrence.
- You must insure that the client has a patent intravenous catheter that is at least 20 gauge.
- You will need the help of another nurse prior to the administration of these packed red blood cells.
- The unit of packed red blood cells should start no more than 1 hour after it is picked up.
- You must remain with and monitor the client for at least 30 minutes after the transfusion begins.
You will need the help of another nurse prior to the administration of these packed red blood cells. Two nurses must check the blood, the doctor’s order, the ABO compatibility and the client’s identity using at least two unique identifiers prior to the administration of this blood.
You must insure that the client has a patent intravenous catheter that is at least 18 gauge and not 20 gauge; you will be using normal saline and a Y infusion set for the administration of the blood because Ringer’s lactate and other intravenous solutions are not compatible with blood; blood should not remain in the client care area for more than 30 minutes so it is important that the nurse is prepared to begin the transfusion shortly after the blood is delivered to the patient care area; and, lastly, the nurse should remain with and monitor the client for at least 15 minutes after the transfusion begins at a slow rate since most serious blood reactions and complications occur shortly after the transfusion begins.
- A percutaneous, non tunneled subclavian catheter
- A peripheral intravenous catheter that is 20 gauge
- A multi lumen implanted tunneled and cuffed central venous catheter
- A peripherally inserted central venous catheter
You would most likely anticipate that this client will be given a multi lumen implanted tunneled and cuffed central venous catheter because this multi trauma client is in need of multiple intravenous therapies such as blood, medications and total parenteral nutrition over an extended period of time.
A percutaneous, non tunneled subclavian catheter would not be the device of preference because percutaneous, non tunneled subclavian catheters are used when short term treatments are anticipated; a peripheral intravenous catheter that is at least 18 gauge is necessary for the administration of blood; and a peripherally inserted central venous catheter would also not be the venous access device of choice for this seriously ill client who will require long term treatments and care.
- 1.5 tablets
- 1.25 tablets
- 1.33 tablets
You have to determine how many tablets the patient will take if the doctor has ordered 200 mg a day and the tablets are manufactured as 150 mg per tablet.
The mathematical rule for this type of calculation is:
Have = Desired Quantity X
This problem is calculated as shown below.
200 mg: X tablets = 150 mg: 1 tablet
200 mg = 150 mg
X tablets 1 tab
You will criss cross multiply the known numbers and then divide this product by the remaining number to solve for X, as below.
200 x 1 = 150 X
200/150 = 1.33 tabs rounded off to 1 1/3 tabs
You have to determine how many mLs the patient will take if the doctor has ordered 10 mg twice a day and there are 12 mg in each mL.
10 mg: X mL = 12 mg: 1 mL
10 mg = 12 mg X mL 1 mL
10 x 1 = 10 X
10/12 = 0.833 mL rounded off to 0.8 mL
You have to determine how many mLs the patient will take if the doctor has ordered 6,500 units of heparin subcutaneously and there are 4,500 units in one mL.
6,500 units: X mL = 4,500 units: 1 mL
6,500 units = 4,500 units X mL 1 mL
6,500 x 1 = 6,500
6,500/4,500 = 1.44 mL which is rounded off to 1.4 mL
To calculate the number of mg that this pediatric client will receive in each dose, you will have to calculate the client’s weight in kg and then determine the total mg for the day after which you will divide the daily dosage by 2 because the order is for two equally divided doses each day.
The steps for this calculation are shown below:
This is how to determine the client’s weight in terms of kg:
48 pounds: x kg = 2.2 pounds: 1 kg
48 pounds = 2.2 pounds x kg 1 kg
48 x 1 = 48
48/2.2 = 21.81 or 21.81 kg
This is how to determine the client’s total daily dosage when the doctor has ordered has ordered 5 mg/kg/day:
21.81 kg x 5 = 109.05 mg per day
This is how to determine the client’s dose for each of the two divided doses:
109.05/2 = 54.53 mg which is rounded off to 55 mg for each of two divided doses.
The first step of this calculation is to calculate the number of mLs, or cc s, per hour and then determine the number of drops per minute. This calculation is done as follows:
1000 ml = 125 mL per hour 8 hrs
The next step is done using this rule that reflects the fact that there are 60 minutes per hour in order to determine the number of mLs per minute .
1 hour = The ordered mL per hour 125 mLs X min 60 min
1 hour = 125 mL X min 60 min
60 x 1 = 60
88/60 = 2.08 mL per minute
Finally, the number of drops per minute is calculated by using the intravenous infusion set’s drop factor by using this rule.
Volume per minute x Drop factor
2.08 x 20 = 41.6 gtts per minute which is rounded off to 42 gtts per minute
With this type of calculation, the amount of normal saline that will be added to a powder in a vial to reconstitute the medication is important, instead, it is the amount of medication that results after the addition of the normal saline. For example, this reconstituted medication yields it is the yield of 12 mg in an mL that is relevant. It is this that will be used in the calculation.
This calculation is done as shown below:
12 mg = 25 mg 1 mL X mL
25 x 1 = 25
25/12 = 2.08 mL which is 2.1 mL rounded off
When the doctor has ordered 1200 mLs of intravenous fluid every 8 hours, you would calculate the number of mLs per hour, as below.
1200/8 = 150 mLs per hour
From 8 am to 12 noon there are 4 hours so:
150 mLs x 4 = 600 mLs
Because you had 600 mLs at 8 am, you should be prepared to hand another intravenous bag because this 600 mLs should all be infused at 12 noon.
- Question the order because Benadryl is an antihistamine and not a sleeping medication.
- Refuse to give the Benadryl because this medication is a stimulant.
- Question the order because Benadryl is contraindicated when the client has a sleep inducement disorder.
- Give the Benadryl because sleep inducement is an accepted off label use of this medication.
You would administer this Benadryl because sleep inducement is an accepted off label use of this medication. When a medication is used for any other than these established and approved uses, this usage is referred to as an “off label use”.
- The “right” verification
- The “right” to refuse
- The “right” documentation
- The “right” client education
The “right verification” is not one of the “Ten Rights of Medication Administration”. The verification of the doctor’s order for a medication is to confirm the right paint, medication, dose, route and time or frequency, it, in itself, is not one of the “10 Rights”.
The “Ten Rights of Medication Administration” are the right, or correct:
- Time or frequency
- Client education
- Documentation
- Right to refuse
- Assessment and
- Gluteus maximus muscle.
- Vastus lateralis muscle.
- Deltoid muscle.
- The sternocledomastoid muscle.
The administration of an intramuscular injection to a neonate should be given in the vastus lateralis, rectus femoris and ventrogluteal muscle sites and not the deltoid or the gluteus maximus muscles because these muscles have not yet developed.
The sternocledomastoid muscle is not an intramuscular injection site.
- A subcutaneous injection site
- The PQRST technique
- The Z track technique
- The sublingual site
You would expect to use to use the Z track technique to administer ferrous sulfate.
Ferrous sulfate IM is given using the Z Track technique to avoid the leakage and dark staining of the injection site with this medication.
Ferrous sulfate is not administered with a subcutaneous injection or using the sublingual route. Lastly, the PQRST method is used to assess pain and not used as a guideline for medication administration.
- 1,5,4,2,3,6
- 4,3,2,6,1,5
- 4,2,5,3,1,6
- 1,5,3,6,4,2
The steps for mixing NPH, the long acting insulin, with regular insulin, the short acting insulin in the correct sequential order are:
- Prep the top of the longer acting insulin vial with an alcohol swab.
- Inject air that is equal to the ordered dosage of the longer acting insulin using the insulin syringe. Do NOT withdraw the longer acting insulin yet.
- Prep the top of the shorter acting insulin with an alcohol swab
- Inject air that is equal to the ordered dosage of the shorter acting insulin using the same insulin syringe.
- Withdraw the ordered dosage of the shorter acting insulin using the same insulin syringe.
- And, then lastly, withdraw the ordered dosage of the longer acting insulin using the same insulin syringe.
- Allow the nurse to administer the injection.
- Ask the nurse to use the vastus lateralis muscle instead.
- Ask the nurse to verify the doctor’s order again.
- Stop the nurse from administering the injection.
You would stop the nurse from administering the injection when you observe that the nurse has palpated the gluteus maximum muscle to determine the correct site. Intramuscular injection sites are determined by using boney landmarks and not by palpating the muscle.
You would not allow the nurse to administer the injection and you would not ask the nurse to use the vastus lateralis muscle instead because nothing indicates the need to do so. Lastly, you would verify the doctor’s order prior to entering the room and preparing to administer the injection and not during the time that the intramuscular site is being identified.
- You have failed to have another nurse witness the 0.8 mLs and the 0.2 mLs of waste.
- You have failed to have another nurse witness the 0.8 mLs of waste.
- You have failed to have another nurse witness the 0.2 mLs of waste.
- You have failed ask another nurse to verify the calculation of the dosage.
You have failed to have another nurse witness the 0.8 mLs and the 0.2 mLs.
All controlled substances are documented on the narcotics record as soon as they are removed, and all controlled substances that are wasted for any reason, either in its entirety or only partially, must be witnessed or documented by the wasting nurse and another nurse. Both nurses document this wasting.
It should not be necessary for you to ask another nurse to verify this calculation; the nurse is accountable and responsible for accurate dosage calculations.
The procedure for this medication reconciliation process is:
2. Compile a list of current medications and other preparations 1. Compile a list of newly prescribed medications 4. Compare the two lists and make note of any discrepancies and inconsistencies 5. Employ critical thinking and professional judgments during the comparisons of the two lists 6. Communicate and document the new list of medications to the appropriate healthcare providers
- The client with heart failure who is receiving Ringer’s lactate
- The client with cancer who is receiving bendamustine
- The client who is receiving potassium supplementation intravenously
- The client who is receiving total parenteral nutrition
The client with cancer who is receiving bendamustine is at greatest risk for extravasation. Extravasation occurs when vesicant and other vein irritating drugs infiltrate into the tissue. In severe cases, extravasation can lead to necrosis and the loss of an affected limb. Bendamustine is a vesicant chemotherapy drug.
Extravasation is not associated with the intravenous administration of Ringers lactate or potassium supplementation intravenously because this solution and medication are not vesicants. These intravenous preparations can lead to infiltration but not extravasation. Lastly, the client who is receiving total parenteral nutrition is at risk for other complications such as infection, but not extravasation.
- Infection: Lowering the limb to promote circulation
- Infiltration: The application of cold to the site
- Extravasation: The aspiration of contents including blood from the IV cannula
- Hematoma: The administration of dexrazonxane
In addition to other interventions, intravenous fluid contents including blood are aspirated from the IV cannula.
Other interventions include immediate cessation of the infusion, elevating the limb, applying warm compresses initially to rid the area of any remaining drug that is in the tissues which is then followed by cool compresses to reduce any swelling, and the administration of an ordered substance specific medication such as dexrazoxane.
One of the interventions for infection include the elevation, not lowering, of the affected limb; infiltration is treated with the application of warm, not cold, compresses and one of the interventions for hematoma is the application of pressure and heat and not the administration of dexrazonxane.
- Assess motor functioning.
- Assess sensory functioning.
- Evaluate responses to a tactile stimulation.
- Evaluate responses to a pain analgesic.
The CRIES scale is used to evaluate the neonate’s response to a pain analgesic; this pain scale is also used to assess pain among neonates.
Observational behavioral pain assessment scales for the pediatric population are used among children less than three years of age. Some of these standardized pediatric pain scales, in addition to the CRIES scale, include the FACES Pain Scale, the Toddler Preschooler Postoperative Pain Scale (TPPPS), the Neonatal Infant Pain Scale (NIPS), the Children's Hospital of Eastern Ontario Pain Scale (CHEOPS), the Faces Legs Activity Cry Consolability Pain Scale (FLACC), the Visual Analog Scale (VASobs) the Observation Scale of Behavioral Distress (OSBD), the COMFORT Pain Scale and the Pre-Verbal Early Verbal Pediatric Pain Scale (PEPPS) that is used with toddlers.
- Opioid Agonist: Dilaudid: Constipation
- Opioid Agonist: Naloxone: Constipation
- Opioid Antagonist: Dilaudid: Anaphylaxis
- Opioid Antagonist: OxyContin: Anaphylaxis
Dilaudid is an opioid agonist that can cause constipation.
Other opioid agonists are codeine, OxyContin, Darvon, Dilaudid, Demerol and Percocet. The side effects and adverse reactions to this classification of drugs include constipation, sedation, nausea, dizziness, pruritus, and sedation, respiratory depression and arrest, hepatic damage, an anaphylactic reaction, circulatory collapse and cardiac arrest.
Opioid antagonists also referred to as opioid receptor antagonists, such as naloxone and naltrexone, can have side effects such as hepatic damage, joint pain, insomnia, vomiting, anxiety, headaches and nervousness.
- Your client may be experiencing a fluid overload.
- Your client may be experiencing an embolus.
- Your client may be hyperglycemic.
- Your client may have an inadvertent pneumothorax.
The client may be experiencing an embolus, which is a complication of total parenteral nutrition. Some of the signs and symptoms of an embolus are chest pain, dyspnea, shortness of breath, coughing, and respiratory distress.
Emboli, secondary to total parenteral nutrition occur when air is permitted to enter this closed system during tubing changes and when a new bottle or bag of hyperalimentation is hung. This complication can be prevented by instructing the client to perform the Valsalva maneuver and the nurse’s rapid changing of tubings and solutions when the closed system is opened to the air.
An inadvertent pneumothorax can occur and become symptomatic during the insertion of the TPN catheter and not four days later.
Other side effects of TPN and their signs and symptoms are listed below.
- Infection: The classical signs of infection including a fever, malaise, swelling and redness at the insertion site, diaphoresis, chilling and pain in the area of the TPN catheter insertion site.
- Fluid overload: Hypertension, edema, adventitious breath sounds like crackles and rales, shortness of breath, and bulging neck veins.
- Hyperglycemia: High blood glucose levels, thirst, excessive urinary output, headache, nausea and fatigue.
- Hypoglycemia: Low blood glucose levels, shakiness, clammy and cool skin, blurry vision, diaphoresis and unconsciousness and seizures.
- Clients are at high risk for infection when they are getting TPN because they are immunocompromised.
- Clients are at high risk for hyperglycemia when they are getting TPN because they are diabetic.
- The client should perform the Valsalva maneuver when the nurse changes the TPN tubing.
- The client should perform the Valsalva maneuver when the nurse changes the TPN dressing.
The client should perform the Valsalva maneuver when the nurse changes the TPN tubing to prevent an embolus which can occur when the tubing is opened to the air while it is being changed.
A mask, not the Valsalva maneuver, is indicated for TPN dressing changes.
Lastly, clients are at risk for infection secondary to TPN because these solutions are high in dextrose and because TPN is an invasive sterile procedure; and clients are at high risk for hyperglycemia when they are getting TPN because these solutions are high in dextrose and not because the client is already a diabetic client.
Physiological Integrity: Reduction of Risk Potential Practice Questions
- Respiratory rate: 32 breaths per minute
- Pulse: 110 beats per minute
- Blood pressure: 55/82
- “The respiratory rate is a little too fast but the other vital signs are normal.”
- “The pulse rate is a little too fast but the other vital signs are normal.”
- “The blood pressure is a little low but the other vital signs are normal.”
- “All of these vital signs are normal for a child that is 2 years of age.”
All of these vital signs are normal for the toddler who is 2 years old. The normal vital signs for the toddler are:
- Respiratory rate: From 20 to 40 per minute
- Pulse rate: From 90 to 140 beats per minute
- Blood pressure: Diastolic from 50 to 80 mm Hg and systolic from 80 to 112 mm Hg
- Pulse: 100 beats per minute
- Blood pressure: 85/55
The respiratory rate is a little too fast for this 5 year old preschool client. The normal respiratory rate for this client should be from 22 to 30 per minute.
The normal pulse rate and blood pressure for the preschool child are from 80 to 110 beats per minute and a diastolic from 50 to 78 mm Hg and a systolic from 82 to 110 mm Hg.
- Pulmonary Artery Systolic Pressure: 22 mm Hg
- Pulmonary Artery Wedge Pressure: 22 mm Hg
- Pulmonary Artery Diastolic Pressure: 10 mm Hg
- Central Venous Pressure: 5 mm Hg
You would report the pulmonary artery wedge pressure of 22 mm Hg because the normal pulmonary artery wedge pressure is from 4 to 12 mm Hg.
The other normal hemodynamic values are:
- Pulmonary Artery Systolic Pressure: 15 to 26 mm Hg
- Pulmonary Artery Diastolic Pressure: 5 to 15 mm Hg
- Central Venous Pressure: 1 to 8 mm Hg
- The need to cleanse the perineal area with circular wipes.
- The need to cleanse the perineal area from the “dirtiest” to the “cleanest”.
- The need to use a new antiseptic wipe for each wipe from the inner to the outer labia.
- The need to use a new antiseptic wipe for each wipe from the outer to the inner labia.
You would instruct your female client to use a new antiseptic wipe for each wipe from the inner to the outer labia.
A principle of asepsis is the cleansing of areas from the cleanest to the dirtiest and NOT the reverse; therefore, the inner labia are cleansed before the outer labia. The female perineal area is prepped with straight strokes and wipes; and the male wipes with a circular pattern around the urinary meatus.
- Turn the finger down so the blood will drop with gravity.
- Wipe off the first drop of blood using sterile gauze.
- Prick the side of the finger using the lancet.
- Prick the pad of the finger using the lancet.
Pricking the pad of the finger using the lancet is NOT a step in the procedure for obtaining a blood glucose sample for testing. Instead, the side of the finger is pricked with the lancet.
The procedure for checking the client’s blood glucose levels in correct sequential order is as follows:
- Verify and confirm that the code strip corresponds to the meter code.
- Disinfect the client’s finger with an alcohol swab.
- Turn the finger down so the blood will drop with gravity.
- Collect the next drop on the test strip.
- Hold the gauze on the client’s finger after the specimen has been obtained.
- Read the client’s blood glucose level on the monitor.
- PaO2: 65 mm Hg
- PaCO2: 40 mm Hg
- Arterial blood pH: 7.39
You would report the client’s PaO2 of 65 mm Hg because it is not within normal parameters and it is also a significant change for the client. The normal partial pressure of oxygen (PaO2) is from 75 to 100 mm Hg.
The other blood gases, above, are within normal limits, as follows:
- Partial pressure of carbon dioxide (PaCO2): 38 - 42 mmHg
- Arterial blood pH: 7.38 - 7.42
- Oxygen saturation (SaO2): 94 - 100%
- Triglycerides: 75 mg/dL
- Total cholesterol: 6.5 mmol/L
- High-density lipoprotein (HDL): 60 mg/dL
- Low-density lipoprotein (LDL): 955 mg/dL
You would report a total cholesterol level of 6.5 mmol/L because this value exceeds the high normal for total cholesterol which is 5.5 mmol/L and the normal range is from 3 to 5.5 mmol/L.
The other lipid levels are normal as follows:
- Triglycerides: 50-150 mg/dL
- High-density lipoprotein (HDL): 40-80 mg/dL
- Low-density lipoprotein (LDL): 85-125 mg/dL
- Albumin: 40 g/L
- Amylase: 40 U/L
- Direct bilirubin: 17 µmol/L
- Total bilirubin: 17 µmol/L
You would report a direct bilirubin level of 17 µmol/L because this value exceeds the high normal for direct bilirubin which is 6 µmol/L and the normal range is from 0-6 µmol/L.
The other gastrointestinal related normal laboratory values are as follows:
- Albumin: 35-50 g/L
- Amylase: 30-125 U/L
- Total bilirubin: 2-20 µmol/L
- A 76 year old female client who has a history of alcohol abuse.
- A 76 year old female client who has a history of radon gas exposure.
- A 64 year old male client who has a history of cigarette smoking.
- A 64 year old male client who has hypotension.
A 64 year old male client who has hypotension is at greatest risk for impaired vascular perfusion.
Other risk factors associated with impaired vascular and tissue perfusion are:
- Hypervolemia
- Hypovolemia
- Low hemoglobin
- An immobilized limb
- Decreased cardiac output
- Impaired oxygen transportation
- Hypoventilation
Alcohol abuse, cigarette smoking and exposures to radon place people at risk for cancer, rather than impaired perfusion.
- A 76 year old female client who has a history of diabetes.
- A 64 year old male client who has a history of impaired oxygen transport.
The client who is at greatest risk for the development of cancer is the 76 year old female client who has a history of alcohol abuse. Data indicates that alcohol abuse can lead to cancer of the liver and other cancers.
Diabetes, a history of impaired oxygen transport and hypotension are risk factors associated with poor tissue perfusion, and not cancer.
- The level of pain among school age children.
- The risk for the impairment of skin integrity.
- Levels of muscular strength.
- Levels of mobility.
The Norton Scale measures the client’s risk for the impairment of skin integrity. The Norton Scale and the Braden Scale are standardized tools to screen clients for their risk of skin breakdown, pressure ulcers and an impairment of skin integrity.
Pain levels among school age children are measured with other standardized pain tools for pediatric clients; and levels of muscular strength and mobility are measured also with other standardized tests and not the Norton Scale.
- Impaired tissue perfusion
Impaired tissue perfusion is an intrinsic, or internal, risk factor that places the client at risk for pressure ulcers.
Pressure, shearing and friction are extrinsic, or external, risk factors that places the client at risk for pressure impaired tissue perfusion.
Other intrinsic risk factors associated with skin breakdown include:
- Poor nutritional status
- A decreased level of consciousness including that which occurs with sedating medications
- Fecal and/or urinary incontinence
- Impaired circulation
- Alterations in terms of the fluid balance
- Altered neurological sensory functioning
- Changes in terms of skin turgor
- Boney prominences
- Inflate the cuff if the cuff is deflated.
- Deflate the cuff if the cuff is inflated.
- Remove the inner cannula of the tube.
- Call the doctor about this airway obstruction.
The first thing that you should do when you insert the suction catheter and you reach a point of resistance is to deflate the cuff when it is inflated and the second thing that you should do is to remove the inner cannula and suction out the mucous plug.
You would not call the doctor because there is an airway obstruction; you should correct this problem with the measures above.
- Maintain the client with NPO status for at least 4 hours prior to this procedure.
- Teach the client about the fact that they may experience muscle flaccidity.
- Teach the client about the fact that they may have a headache after the ECT.
- Maintain the client on continuous hemodynamic monitoring after the ECT.
You would teach the client about the fact that they may have a headache after the ECT. Other components of the teaching about the aftermath of the procedure that the client should know about include the fact that the client may have muscle soreness, not muscle flaccidity, confusion, amnesia and hypertension.
The client should be maintained as NPO for at least 6 hours before ECT; and it is not necessary to maintain the client on continuous hemodynamic monitoring after the ECT, however, the client’s vital signs should be monitored.
- Strnagulation
- Skin breakdown
- Skin pallor
The neurological complication can occur when a vest restraint is too tight around the client’s body is numbness and tingling that, unless corrected, can lead to neurological damage.
Strangulation, skin breakdown and skin pallor can also occur when a restraint is too tight, however, these restraint complications are respiratory, integumentary system and circulatory system complications rather than neurological complications.
- The appearance of petechiae
- Aplastic anemia
- The appearance of thrombophlebitis
- Elevated platelets
The appearance of petechiae is a sign of thrombocytopenia which is a low platelet count. Other signs and symptoms include purpura, easy bruising, epistaxis, and spontaneous hemorrhage and bleeding.
Thrombocytopenia can occur as the result of several disorders and therapeutic treatments and interventions including aplastic anemia, HIV infection, a genetic disorder, cancer, particularly cancer that affects the bones, some viral pathogens like those that cause mononucleosis, as well as from therapeutic radiation therapy, chemotherapy and some medications such as Depakote.
- Pneumothorax
The complication that you should be aware of during the immediate post-operative period of time after a thoracentesis is a pneumothorax.
The signs and symptoms of pneumothorax and hemothorax include dyspnea, chest pain, shortness of breath and pain. The treatment of a pneumothorax includes the correction of the underlying cause whenever possible and the placement of a chest tube to remove the blood and/or air in the pleural space which will re-expand the affected lung and recreate the negative pressure of the pleural space.
Infection would not be evident during the immediate post-operative period; and, aspiration is not a complication of a thoracentesis.
- The client’s posterior tibia pulse is Grade B
- The client’s posterior tibia pulse is Grade C
- The client’s posterior tibia pulse is 1
- The client’s posterior tibia pulse is 2
You would document this finding as “The client’s posterior tibia pulse is 1”.
The strength, volume and fullness of the peripheral pulses are categorized and documented as follows:
- 0: Absent pulses
- 1: Weak pulse
- 2: Normal pulse
- 3: Increased volume
- 4: A bounding pulse
Grades and grading are not used in reference to pulses.
- The Lazarus Cognitive Appraisal Scale
- The Hamilton Rating Scale
- The McGill Scale
- The Rancho Los Amigos Scale
The tool or scale that you would use for a focused neurological assessment of your client is the Rancho Los Amigos Scale.
Levels of consciousness, which is part of a complete focused neurological assessment, can be determined and measured by using the standardized Glasgow Coma Scale for adults and children or the Rancho Los Amigos Scale. The Rancho Los Amigos Scale determines the patient’s level of awareness and functioning which can range from a 1 to an 8 when a 1 is the complete lack of all responsiveness to all stimulation and an 8 is when a patient is fully alert, oriented, appropriate and purposeful.
The McGill Pain Assessment is used to assess pain levels; the Lazarus Cognitive Appraisal Scale is used to assess levels of stress and coping; and the Hamilton Rating Scale is used to measure and assess depression.
- A lack of zinc
- A lack of vitamin E
- High iron levels
- High phosphorous levels
A lack of zinc, copper, iron and vitamins C and A are risks associated with impaired and delayed wound healing.
Other risk factors that impede wound healing are:
- Advancing age
- Nutritional status
- Some poor lifestyle choices
- Some medications
- Some diseases and disorders
- “The client is having anesthesia awareness which is not good.”
- “This often happens during stage 2 of general anesthesia.”
- "The client needs more general anesthesia.”
- “The client is having a seizure.”
You should respond to this student nurse by stating, “This often happens during stage 2 of general anesthesia.”
Stage 2 of general anesthesia, often referred to as the Excitement Stage, is characterized with uncontrollable muscular activity, irregular respirations, an irregular cardiac rhythm, and, at times, vomiting. This stage does not indicate the need for more general anesthesia.
Anesthesia awareness, which is a rare complication of general anesthesia, is the lack of amnesia during surgery when the client remembers events during surgery and, at times, they remember the pain.
Lastly, there is no evidence in this question that the client is having a seizure.
- Surgical site marking
- Medication reconciliation
- A neutral zone for sharps
Medication reconciliation prevents medication errors and other complications associated with medications and not a way to reduce surgical risks.
Surgical marking, time outs that are done after surgical site marking is done, and a neutral zone for sharps do reduce surgical risks such as wrong site surgery, wrong patient surgeries and sharps injuries.
Physiological Integrity: Physiological Adaptation Practice Questions
- Exclude pregnant visitors from the client’s room.
- Place the client in a negative pressure room.
- Have all visitors wear protective masks and boots.
- All of the above
You would exclude all pregnant visitors from the client’s room in order to protect the pregnant woman’s developing fetus. Brachytherapy is internally placed radioactive material to treat clients who are affected with tumor and cancer of the prostate, lungs, esophagus, cervix, endometrium, rectum, breast, head and neck.
Special radiation precautions are initiated when a client is receiving brachytherapy in order to protect visitors and health care staff from the harmful effects of the radiation. Some of the other special internal radiation precautions include:
- The minimization of the duration of time that health care providers are in the client’s room to deliver care and services to the client
- The placement of the client receiving internal radiation in a private room. A negative pressure room is not indicated for this client.
- The prohibition of the client’s activities outside of their room
- The initiation of complete bed rest for the client until the treatment is discontinued
- The provision of education to the family members and other visitors that includes information about their need to limit the time of their visits to at least less than 1 hour, to stay at least 6 feet away from the client
- The need for health care staff to minimize the amount of time spent in the room, to decline to enter the room if they are pregnant, to retain all supplies and equipment including things like bed linens in the client’s room until they are deemed safe for disposal by a person who is competent to make this decision, and how and when to report concerns about the client’s treatment such as when implanted seeds inadvertently leave the client’s body.
- Oral dryness
Fibrosis is an adverse effect to therapeutic radiation therapy.
Radiation fibrosis can affect bones, nerves, ligaments, muscles, blood vessels, tendons, and the heart in addition to the lungs. Fibrosis occurs as the result of abnormal fibrin and protein accumulation within normal irradiated tissue.
Alopecia, and oral dryness which is also referred to as xerostomia, are side effects and complications to radiation, but not adverse effects.
Other side effects, complications and adverse effects associated with therapeutic radiation therapy are:
- Skin damage
- Damage to the mucosa
- Dental caries and oral infections
- Nausea and vomiting
- Bone marrow suppression and immunosuppression
- Radiation pneumonia
- Placing the client in the Trendelenburg position
- Monitoring the color of the stools
- Using a Hoyer lift for patient transfers
- Monitoring the arterial blood gases
You would monitor the color of the stools for the client who is receiving phototherapy. Phototherapy is used to treat psoriasis, but it is most commonly employed for the treatment of neonatal hyperbilirubinemia and jaundice which can occur among both full term and pre term infants.
You would also monitor and document the client’s:
- Skin for changes in color that may indicate an increase or decrease in the amount of bilirubin in the client’s blood
- Laboratory bilirubin levels to determine whether or not the client’s bilirubin levels are decreasing as the result of the phototherapy
- Volume, color and characteristics of the stool because phototherapy can lead to frequent, loose stools as well as a color change to green colored stools
- Hypokalemia: Hypermagnesemia
- Hyponatremia: Dehydration
- Hyperkalemia: Ketoacidosis
- Hypercalcemia: Hypoparathyroidism
Ketoacidosis is a risk factor for hyperkalemia.
The risk factors for the other electrolyte disorders above are listed below.
- Hypokalemia: Diarrhea, vomiting, and diaphoresis as well as some medications like diuretics and laxatives, and with other disorders and diseases such as ketoacidosis. Hypermagnesemia is not a risk factor for hypokalemia.
- Hyponatremia: Thyroid gland disorders, cirrhosis, renal failure, heart failure, pneumonia, diabetes insipidus, Addison’s disease, hypothyroidism, primary polydipsia, severe diarrhea or vomiting cancer, and cerebral disorders. Dehydration is a risk factor associated with hypernatremia, not hyponatremia.
- Hypercalcemia: Hyperparathyroidism, not hyperparathyroidism, some medications such as thiazide diuretics and lithium, some forms of cancer such as breast cancer and cancer of the lungs, with multiple myeloma, Paget’s disease, non weight bearing activity and elevated levels of calcitriol as occurs with sarcoidosis and tuberculosis.
- Hypernatremia: Hepatic failure
- Hypocalcemia: Vitamin A deficiency
- Hypermagnesemia: Cushing’s disease
- Hypomagnesemia: Crohn’s disease
Crohn’s disease is a risk factor for hypomagnesemia.
Other electrolyte disorder risk factors include:
- Hypernatremia: Dehydration, renal failure, hyperglycemia and Cushing’s disease
- Hypocalcemia: Vitamin D deficiency, Crohn’s disease, sepsis and pancreatitis
- Hypermagnesemia: Addison’s disease, renal failure, diabetic ketoacidosis and dehydration
- Phosphate: From 0.81 to 1.45 mmol/L.
- Chloride: From 60 to 110 mEq/L.
- Calcium: From 6.5 - 10.6 mg/dL.
- Potassium: From 3.7 to 7.2 mEq/L.
The normal level of phosphate is from 0.81 to 1.45 mmol/L.
The other normal levels for these electrolytes are:
- Chloride: From 97 to107 mEq/L.
- Calcium: From 8.5 - 10.6 mg/dL.
- Potassium: From 3.7 to 5.2 mEq/L.
- Idioventricular Rhythm
- Bundle Branch Block
- Sinus bradycardia
- Atrial Flutter
Sinus bradycardia is a sinus rhythm that is like the normal sinus rhythm with the exception of the number of beats per minute. Sinus bradycardia has a cardiac rate less than 60 beats per minute, the atrial and the ventricular rhythms are regular, the P wave occurs prior to each and every QRS complex, the P waves are uniform in shape, the length of the PR interval is form 0.12 to 0.20 seconds, the QRS complexes are uniform and the length of these QRS complexes are from 0.06 to 0.12 seconds.

- Atrial flutter
- Supraventricular Tachycardia
- Premature Atrial Contractions
Atrial flutter, which is a relatively frequently occurring tachyarrhymia; this cardiac rhythm is characterized with an rapid atrial rate of 250 to 400 beats per minute, a variable ventricular rate, a regular atrial rhythm, a possibly irregular ventricular rhythm, the P waves are not normal, the flutter wave has a saw tooth look (f waves), the PR interval is not measurable, QRS complexes are uniform and the length of these QRS complexes are from 0.06 to 0.12 seconds.
- Torsades de Pointes
- Accelerated Idioventricular Arrhythmia
- First Degree Atrioventricular Heart Block
- Supraventricular tachycardia
Supraventricular tachycardia, simply defined is all tachyarrhythmias with a heart rate of more than 150 beats per minute.
The atrial and ventricular cardiac rates are from 150 to 250 beats per minute, the cardiac rhythm is regular, the p wave may not be visible because it is behind the QRS complex, the PR interval is not discernable, the QRS complexes look alike, and the length of the QRS complexes ranges from 0.06 to 0.12 seconds.
- Third Degree Heart Block
- Second-Degree Atrioventricular Block, Type II
- Ventricular fibrillation
The two types of ventricular fibrillation that can be seen on an ECG strip are fine ventricular fibrillation and coarse ventricular fibrillation; ventricular fibrillation occurs when there are multiple electrical impulses from several ventricular site. This results in erratic and uncoordinated ventricular and/or atrial contractions.
You would instill 250 mLs of irrigating solution after each suctioning of the nasogastric tube. The typical amount of irrigating solution is from 20 mLs to 300 mLs.
- The compression of the renal medulla.
- Syncope and dizziness of unknown origin.
- Pressure on the vena cava which is a major vein in the body.
- Pressure on the vena cava which is the largest artery in the body.
You should explain that superior vena cava syndrome is pressure on the vena cava which is a major vein, not an artery, in the body that carries blood from the systemic circulation to the right atrium of the heart. This pressure on the superior vena cava prevents the normal return of the body’s circulating blood to the heart.
The signs and symptoms of superior vena cava syndrome include tachypnea, dyspnea, venous stasis, a loss of consciousness, edema, seizures, respiratory and/or cardiac arrest and not syncope of unknown origin. This is a life threatening medical emergency.
- Hypovolemic shock
- Septic shock
- A dissected thoracic aortic aneurysm
You would most likely suspect that this client is affected with a dissected thoracic aneurysm. Thoracic aorta rupture and dissections can present with symptoms that can include shortness of breath, dysphagia, dyspnea, coughing, and pain in the chest, arms, jaw, neck, and/or back.
The signs and symptoms of hypovolemic shock vary according to the stage of the shock; some of the signs and symptoms include hypotension, tachycardia, a lack of tissue perfusion, hyperventilation, decreased cardiac output, decreased urinary output, oliguria, anuria, metabolic acidosis, increased blood viscosity, and multisystem failure.
The signs and symptoms of septic shock include the classical signs of infection in addition to hypotension, confusion, metabolic acidosis, respiratory alkalosis, abnormal breath sounds like crackles and rales, a widened pulse pressure, and decreased cardiac output.
- Part of the intestine slides into another part of the intestine.
- The appendix ruptures.
- An ileostomy stoma retracts below the abdominal surface.
- Lungs are infiltrated.
Intussusception occurs when a part of the intestine slides into another part of the intestine. This medical emergency can lead to poor perfusion to the intestine.
The signs and symptoms of intussusception include knee to chest posturing, abdominal pain, bloody stool, fever, constipation, vomiting and diarrhea.
A ruptured appendix occurs when an infected appendix ruptures; a stoma retraction occurs when an ileostomy stoma retracts below the abdominal surface; and pneumonia occurs when the lungs become infiltrated.
- The administration of a thrombolytic medication
- The administration of hyroxyurea
- Placing the client in the lithotomy position
You would expect to administer hydroxyurea which prevents the sickling of the client’s red blood cells. You would not administer a thrombolytic medication; however, you would likely administer analgesic medications for the pain associated with the sickle cell crisis.
The lithotomy position is used for procedures involving the pelvis, including gynecological examinations; and the Trendelenburg position is used when the client is in shock and with significant hypotension.
- Perform the Valsalva maneuver
- Encourage the person to continue coughing
- Perform the Heimlich maneuver
- Begin CPR and prepare for ACLS measures
You would encourage the person to continue coughing because this person has a partial airway obstruction.
You would perform the Heimlich maneuver when the person has a complete airway obstruction. CPR and ACLS may be necessary later, but not now as based on the fact that the person only has a partial airway obstruction. Lastly, the Valsalva maneuver is done when one exerts pressure against resistance.
- Trichomoniasis
- Staphylococcus aureus
- Neisseria gonorrhoeae
Pelvic inflammatory disease is most often caused by the Neisseria gonorrhoeae and Chlamydia trachomatis pathogens; and it most often occurs as the result of untreated salpingitis, pelvic peritonitis, a tubo ovarian abscess and/or endometritis.
Unlike Neisseria gonorrhoeae, trichomoniasis and infections caused by E. coli and Staphylococcus aureus are not associated with the onset of pelvic inflammatory disease which can lead to infertility, increased risk for ectopic pregnancies, sepsis, septic shock and death when left untreated.
- Adaptive immunity
- Passive natural immunity
- Active natural immunity
- Active artificial immunity
The type of immunity occurs when a person has an infectious, communicable disease like the measles is active natural immunity.
Active immunity occurs as the result of our bodily response to the presence of an antigen, with the development of antibodies. Active immunity can be both natural and artificial. Natural active immunity occurs when the body produces antibodies after the client is infected with a pathogen; and artificial active immunity occurs when the body produces antibodies to an immunization vaccine such as those for pneumonia and a wide variety of childhood infectious diseases.
Adaptive immunity is the acquisition of antibodies or activated T cells in the body. Passive immunity occurs when an antibody is introduced into the body by either natural or artificial means. Passive natural immunity occurs when the fetus and neonate receive immunity as a natural process through the placenta; and passive artificial immunity occurs when the client receives an injection of immune globulin.
- The incubation stage
- The prodromal stage
The prodromal stage, or phase, of the infection process is characterized with general malaise, joint and muscular aches and pains, anorexia, and the presence of a headache. The prodromal stage begins with the onset of symptoms and this stage is characterized with the replication and reproduction of the pathogen.
The incubation stage is asymptomatic; the illness stage is the period of time that begins with continuation of the signs and symptoms and it continues until the symptoms are no longer as serious as they were before; and the convalescence stage is the period of recovery during which time the symptoms completely disappear.
- They are not as effective as regular defibrillators.
- They are replacing regular defibrillators in acute care settings.
- Only BLS certified people in the community should use them.
- They can be easily used by people with no healthcare experience.
Automated external defibrillators can be easily used by people with no healthcare experience. Automated external defibrillators are simple to use and there is no need to be able to recognize cardiac arrhythmias or interpret cardiac rhythm strips. Automated external defibrillations are intended to be used by the general public without any healthcare or nursing knowledge of experience; therefore, they are not restricted to only those BLS certified.
Although they are highly effective, they are not replacing the standard defibrillators in the acute care setting.
- Episiotomy extension related to a forceps delivery
- Respiratory depression related to NSAIDs
- Hemothorax related to a latex allergy
Maternal trauma, lacerations, pelvic floor damage, bleeding and an inadvertent extension of the episiotomy to the anus when a forceps delivery of a new born is done.
Respiratory depression can occur as the result of narcotic analgesics such as morphine, and not NSAIDs; pneumothorax and hemothorax can occur as the result of an inadvertent perforation during invasive procedures such as the placement of a total parenteral nutrition catheter and a thoracentesis; and the signs and symptoms of a latex allergy include tachycardia, hypotension, dyspnea, chest pain tremors, and anaphylactic shock, not respiratory depression.
- Help Center
- Nursing Career Guide
- Premium Login
- Pass the first time, guaranteed
Free NCLEX Practice Questions: Pass Your Exam with Confidence
Ace your Next-Gen NCLEX-RN exam with the Nurse Plus Academy! Expert-authored questions mirror the actual test format and content, come with detailed rationales, and are organized by NCLEX topics, ensuring you have the knowledge and confidence to succeed on exam day.
Master your 2024 NCLEX-PN exam with ultra-realistic practice questions tailored just for you. Dive into our computer-adaptive Exam Simulator. Gain strategic insights and test-taking tactics for your nursing licensure exam.
Welcome to Nurse Plus Flashcards, a proven tool to enhance your NCLEX exam preparation. Utilize our flashcards to improve recall and focus on areas that need further study.
- Physiological
- Psychosocial
Health Promotion
Safe and effective care.
- Exam Simulator
Basic Care & Comfort
Basic Care & Comfort 1
Questions cover Medical Emergencies, Changes/Abnormalities in Vital Signs, Arterial Blood Gases, Potential for Complications of Procedures, and Patient Positions.
Basic Care & Comfort 2
Questions cover Total Parenteral Nutrition, Intravenous Therapy, Laboratory Values, Blood and Blood Products, Alterations in Body Systems.
Basic Care & Comfort Marathon
This Marathon is your last step before moving on to the next level. It contains all 114 questions from the Basic Care & Comfort tests and will cycle through your missed questions until you answer each one correctly.
Meet Our Experts
At Nurse Plus Academy, your success is guided by leading professionals. Our Nursing Adviser, Winona Suzanne Ball , RN, MHS from Governors State University, IL, brings 30+ years of clinical expertise and educational acumen to our curriculum design. Every piece of content is meticulously reviewed by Steven Litvintchouk , our full-time copyeditor and researcher, and a respected Full Member of the American Copy Editors Society (ACES).
Pharmacological & Parenteral Therapies
Pharmacological & Parenteral Therapies 1
Covers must-know topics like Pathophysiology, Unexpected Response to Therapies, Dosage Calculation, and Pharmacological Pain Management.
Pharmacological & Parenteral Therapies 2
The topics covered in this NCLEX-RN practice test include Medication Administration, Hemodynamics, Pathophysiology, and Lab Values.
Pharmacological & Parenteral Therapies 3
This members-only question set covers dosage calculations, intravenous drip rates, medication allergies, side effects, and therapeutic drug levels.
Pharmacological & Parenteral Therapies 4
Sample questions on insulin administration, dosage calculations, laboratory values, IV solutions, over-the-counter (OTC) medications, and client education.
Drug Dosage Calculation Test
Here are 50 Pharmacological Calculation problems: dosages, IV rates, drug reconstitution, common measurements, and percentage strength.
Pharmacological & Parenteral Therapies Marathon
Contains all 248 questions from the Pharmacological & Parenteral Therapies tests and will cycle through your missed questions until you answer each one correctly.
Reduction of Risk Potential
Risk Potential Reduction 1
Test your knowledge on arterial blood gases (ABGs), laboratory values, breath sounds, blood administration, and client education.
Risk Potential Reduction 2
This practice test asks about post-operative care, abnormal laboratory values, inserting nasogastric (NG) tubes, and client education.
Risk Potential Reduction 3
Answer questions on emergency interventions, Glasgow Coma Scale, infant and pediatric care, and personal protective equipment (PPE).
Reduction of Risk Potential 4
Take this practice test to answer questions on arterial blood gas values, risk factors for developing a deep vein thrombosis, pre-operative education, and measuring kidney function.
Reduction of Risk Potential Marathon
Your last step before proceeding to the next section. It contains all 207 questions from the Reduction of Risk Potential tests and will cycle through your missed questions until you answer each one correctly.
Physiological Adaptation
Physiological Adaptation 1
This practice test covers electrocardiogram (ECG) rhythm strips, disease pathophysiology, respiratory system interventions, and nutrition education.
Physiological Adaptation 2
Questions about neurological disorders, cardiac conditions, components of an ECG tracing, deep vein thrombosis, and pediatric issues.
Physiological Adaptation 3
Here are questions about post-operative care, drainage methods, prenatal and delivery situations, and Emergency Department client cases.
Physiological Adaptation 4
This practice test has questions about Nagele’s Rule, laboratory results, signs & symptoms of disorders, and ECG interpretation.
Physiological Adaptation Marathon
Your last step before proceeding to the next section. It contains all 198 questions from the Physiological Adaptation tests and will cycle through your missed questions until you answer each one correctly.
Psychosocial Integrity
Psychosocial Integrity 1
Topics covered in this practice test include Coping Mechanisms, Sensory/Perceptual Alterations, Therapeutic Medications, Cultural Awareness and Mental Health Concepts.
Psychosocial Integrity 2
Some of the psychosocial topics covered by these practice questions include Therapeutic environment, Behavioral interventions, Depression, Substance abuse and Mental health disorders.
Psychosocial Integrity 3
Some of the NCLEX topics covered by these practice questions include Mental health concepts, Behavioral interventions, Substance abuse disorders, Abuse/Neglect and Sensory/Perceptual alterations.
Psychosocial Integrity 4
Psychosocial Integrity 5
Some of the NCLEX topics covered by these questions include Mental health concepts, Behavioral interventions, Substance abuse disorders, Abuse/Neglect and Sensory/Perceptual alterations.
Psychosocial Integrity Marathon
Psychosocial Marathon is your last step before moving on to the next level. It contains all 215 questions from the Psychosocial Integrity tests and will cycle through your missed questions until you answer each one correctly.
- Health Promotion and Maintenance
Health Promotion and Maintenance 1
In this test, there are 45 questions that include antenatal care, self-care, developmental stages, aging process and newborn care.
Health Promotion and Maintenance 2
To help you prepare, this practice test has 45 questions covering developmental stages and transitions, disease prevention, intranatal care, high-risk behaviors and health promotion.
Health Promotion and Maintenance 3
In this practice test, you will find questions in the following subcategories: high-risk behavior, intranatal care, lifestyle choices, developmental stages and physical assessment.
Health Promotion and Maintenance 4
The 45 questions in this practice test include the following subcategories: self-care, intra- and postpartum care, aging process, lifestyle choices and physical assessment.
Health Promotion and Maintenance 5
The subcategories included in this Health Promotion and Maintenance practice test are developmental stages and transitions, aging process, prenatal care, health promotion/disease prevention and newborn care.
Health Promotion and Maintenance Marathon
Health Promotion and Maintenance Marathon is your last step before moving on to the next level. It contains all 225 questions from the Health Promotion and Maintenance tests and will cycle through your missed questions until you answer each one correctly.
Management of Care
Management of Care 1
Questions cover prioritizing and delegating client care, legal issues, informed consent, and role of the case manager.
Management of Care 2
Topics in this practice test include scope of practice, client advocacy, legal terms, ethics, and informed consent.
Management of Care 3
Challenges you on quality improvement, chain-of-command, HIPAA, legal aspects of informed consent, and ethics.
Management of Care Marathon
Your last step before moving on to the next section. It contains all 157 questions from Management of Care tests and will cycle through your missed questions until you answer each one correctly. When you miss a question, you’ll see it again at the very end.
What’s Your Time and Sanity Worth?
Sure you can study the dusty textbooks, but they don’t give you a pass guarantee. We do. Pass your NCLEX exam using our fast and efficient method, or it’s free.
Safety & Infection Control
Safety & Infection Control 1
Topics include fall risks, trauma situations, needlesticks, isolation protocols, and clarifying HCP medication orders.
Safety & Infection Control 2
Covers home safety, nursing care outside acute settings, client identification, hand hygiene, and medication issues.
Safety & Infection Control 3
Questions cover pediatric situations, fire safety procedures, disease transmission, client education, and nursing assessment.
Safety & Infection Control Marathon
Your last step before moving on to the next section. It contains all 155 from Safety & Infection Control tests and will cycle through your missed questions until you answer each one correctly.
Next Generation NCLEX
Extended Multiple Response (EMR)
The extended multiple-response items allow candidates to choose more than one answer. It is similar to the traditional NCLEX multiple response; however, there are more answer options.
Extended Drag and Drop
Extended drag-and-drop items ask candidates to move or place responses into answer spaces. This type is similar to the current NCLEX ordered response question format, except that they may not use all the answer choices.
Cloze (Drop-Down)
Cloze (drop-down) items ask candidates to select an option from a drop-down list. On the NGN, there may be more than one drop-down list in the cloze question.
Enhanced Hot Spot (Highlighting)
Enhanced hot spot items let candidates choose their answers by highlighting certain words or phrases. For example, they may read a nursing note, medical history, or medication record and then be asked to highlight areas or lines that answer the test question.
Matrix Multiple Choice (Matrix MC)
Matrix grid items allow candidates to select multiple answers on a chart. Each row or column may require a response. This question type may give a scenario with client data and then require test-takers to judge the findings by checking appropriate boxes in a supporting table.
Matrix Multiple Response (Matrix MR)
Case Studies 1-2
Each case study consists of a clinical scenario and six questions requiring candidates to make multiple decisions.
Case Studies 3-4
Case Studies 5-6
Case Studies 7-8
Case Studies 9-10
Case Studies 11-12
Select All That Apply (SATA) questions
Select All That Apply Test 1
SATA nursing questions require you to select all answer choices that apply from among five or six answer options. You must get all options correct (even if you miss one, it is considered wrong; there’s no partial credit).
Select All That Apply Test 2
Select All That Apply Test 3
Select All That Apply Test 4
Select All That Apply Test 5
Select All That Apply Test 6
Select All That Apply Test 7
One more set of SATA (select-all-that-apply) questions — one of the hardest NCLEX exam preparation question types. These are the dreaded “multiple response” questions where you’ll be required to select all answer choices that apply.
NCLEX-RN Exam Simulator
Just like the real NCLEX-RN exam! This NCLEX Simulator mimics the experience and the actual algorithms used on the official NCLEX® exam. It uses computer adaptive testing (CAT) to measure the competencies needed to perform safely and effectively as a newly licensed, entry-level nurse. You’ll get different questions based on how you answered previous questions. You’ll answer a minimum of 85 questions to a maximum of 150 questions.
Pediatric Nursing
Pediatric Test 1
This free test covers routine wellness checks, SIDS, FTT, and more.
Pediatric Test 2
25 questions on Infant Mortality Rate, immunizations, and CoA.
Pediatric Test 3
Topics covered: developmental stages, childhood viral infections, and more.
Pediatric Test 4
Covers must-know topics like parent education, home assessment, and Erikson’s stages of psychosocial development.
Pediatric Test 5
Topics covered include temper tantrums, child’s nutritional needs, and discharge instructions.
Pediatric Test 6
Covers developmental delays, nurse’s best responses in certain situations, and congenital birth defects.
Pediatric Test 7
This members-only test covers bedwetting, assessing neonates, and overdose treatments.
Pediatric Test 8
Questions on parent education, routine check-ups, and anxiety in children.
Pediatric Test 9
Contains 25 questions on interventions, pathologies, and proper dosages.
Pediatric Test 10
Questions about diet recommendations, developmental delay, and administering medication.
Pediatric Test 11
Topics covered: certain age characteristics, pain rating scale, and developing a care plan.
Pediatric Test 12
Includes questions on infant routine exams, respiratory assessments, and appropriate interventions.
Pediatric SATA Test
This test contains 33 Select-All-That-Apply (SATA) questions, where multiple answer options are possible.
NCLEX-PN Exam Simulator
- Physiological Integrity
This practice test covers client nutrition, post-operative care, client with a colostomy, post-mortem care, and nursing assessment.
Pharmacological Therapies
Questions include dosage calculations, drug interactions, insulin administration, adverse effects, blood transfusions, and client education.
Drug Dosage Calculations
40 Pharmacological Calculation problems: dosages, IV rates, drug reconstitution, common measurements, and percentage strength.
Topics include vital sign assessment, laboratory values, disease risk factors, client positioning, and neurovascular complications.
This practice test covers pressure ulcers, chronic disorders, acute and trauma situations, client education, and health promotion.
Physiological Integrity Marathon
Contains all 280 questions from the Physiological Integrity tests and will cycle through your missed questions until you answer each one correctly.
This practice test includes questions about therapeutic responses to client anxiety, developmental stages of life, cultural considerations, and substance abuse.
This NCLEX-PN practice test includes questions about Alzheimer’s Disease and dementia, mental health terms and situations, and therapeutic interventions by the nurse.
Topics covered in this NCLEX-PN practice test include therapeutic responses to major life events, different types of abuse, and mental health terms.
Psychosocial Marathon is your last step before moving on to the next level. It contains all 95 questions from the Psychosocial Integrity tests and will cycle through your missed questions until you answer each one correctly.
This practice test includes questions about Developmental Stages, Client Teaching in Clinical and Community Settings, and Common Health Conditions.
This NCLEX-PN practice test has questions about Clinical and Community Education, Nutrition, Preventive medicine, Ethics, and Lifestyle.
Health Promotion and Maintenance Marathon is your last step before moving on to the next level. It contains all 66 questions from the Health Promotion and Maintenance tests and will cycle through your missed questions until you answer each one correctly.
Coordinated Care
Topics for this test include client prioritization, delegation, informed consent, ethics, HIPAA Privacy Act, and Advance Directives.
Questions cover disease transmission, preventing infections, fire safety, hand hygiene, client allergies, and CDC precautions.
Safe and Effective Care Environment Marathon
Safe and Effective Care Environment Marathon is your last step before moving on to the next level. It contains all 121 questions from the Safe and Effective Care Environment tests and will cycle through your missed questions until you answer each one correctly.
SATA (Select All That Apply) Test 1
SATA (Select All That Apply) Test 2
SATA (Select All That Apply) Test 3
SATA (Select All That Apply) Test 4
SATA (Select All That Apply) Test 5
Just like the real NCLEX-PN exam! This NCLEX Simulator mimics the experience and the actual algorithms used on the official NCLEX® exam. It uses computer adaptive testing (CAT) to measure the competencies needed to perform safely and effectively as a newly licensed, entry-level nurse. You’ll get different questions based on how you answered previous questions. You’ll answer a minimum of 85 questions to a maximum of 150 questions.
Safe & Effective Environment
Terms & abbreviations.
Over 80 questions for the state NCLEX exam
Over 100 questions for the state NCLEX exam
Over 70 questions for the state NCLEX exam
- Safe and Effective Care Environment
Free & Premium Test Practice
More effective than traditional nursing classes. Every practice test is based on authentic exam questions, and you can study at your own pace. We'll shuffle the questions every time you restart a test.
No Registration or Login Required
In the free mode, your test progress is saved without an account, even if you close your browser. No usernames or passwords to remember - just frictionless NCLEX training.
Just Like the Real Test
See if you're ready for the real thing with the computer adaptive NCLEX Simulator that mimics the actual algorithms used on the NCLEX® exam. Same number of questions and format as the RN exam.
7 Steps to Passing
Start preparing for your National Council Licensure Examination (NCLEX) about 3 or 4 months before the exam.
Take several NCLEX practice tests per day (between 80 and 100 questions) to keep you focused.
Make sure you cover all the topics and skills that will appear on the official exam.
Study to learn and understand, not to memorize. Read every practice question carefully before selecting the answer.
Take notes. Taking notes on the questions you need to study will reinforce your learning.
Read the rationales for the correct answers. You likely remember all this from your nursing school!
If you don’t know the answer right away, try to eliminate one or two of the choices.
How it works
The best way to study for your examination is to practice answering questions similar to those you’ll find on the actual test.
Our questions are based on the same categories that are included in the official exam provided by the National Council of State Boards of Nursing (NCSBN):
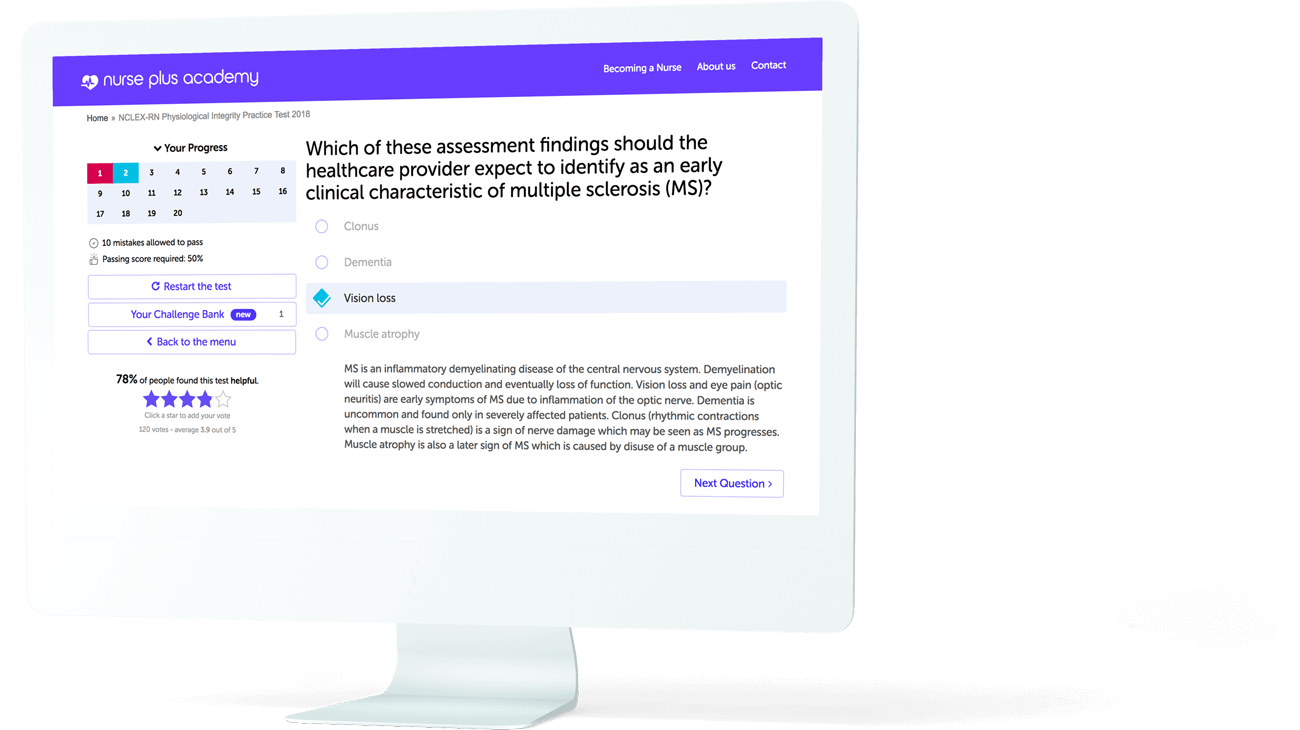
Maximize your study time
You can take our practice tests as many times as you like. Study to learn and understand, not to memorize.
Like flashcards, only easier
Each time you restart a practice test, the questions and their possible answers are randomly shuffled so that you are learning facts, not the order of the questions.

Scientifically proven
Research has shown that studying in the same way that you’ll be tested can increase your self-assurance as well as your ability to answer the test questions.
We’ve designed our practice tests to duplicate the exam experience so that it becomes familiar to you.
Our questions cover all the topics and skills that appear on the official 2024 Registered Nurse and Practical Nurse exams.
Nurses are angels in comfortable shoes
Smart hints.
Short tips, available right when you need them. You decide whether to see them. So you'll know all about things like semi-fowler's position or Erikson's stages .
Explanations
Detailed rationales for the correct answers. Displayed not only when you make a mistake but also when you answer correctly, so you remember it better.
NCLEX Exam Simulator
Designed to simulate the actual NCLEX-RN experience in every way. The most efficient way to practice for the real exam.
Immediate Feedback
No need to wait until you reach the end of the test to see if your answer is right.
If you make a mistake, we'll let you know right away.
Frequently asked questions
If I’m not sure about which option is best, should I guess?
Random guessing on the NCLEX will lower your score. If you don’t know the answer right away, try to eliminate one or two of the choices. On Nurse.plus practice tests, if you’re not sure, or if the question has new information that you haven’t seen before, click on the Hint button below the fourth answer option. You’ll get a clue to help you figure out the correct answer.
How can the Nurse Plus Academy help me study?
Research shows that practice tests are valuable tools in helping you prepare to sit for your NCLEX. They can decrease anxiety about test-taking: the more practice tests you take, the better you become at reading the questions and developing a strategy for choosing the best answer. They also identify your areas of strength and weakness. We recommend a regular study schedule, starting 2-3 months before your examination. In addition to practice testing, we offer a Nursing Terminology section where you can see definitions for the most popular NCLEX terms such as Sims position , rule of nines , 12 cranial nerves or what normal saline and d5w are .
When do I get the score for my practice test?
Your score is constantly displayed. Before you begin, the numbered grid is grey. As you take each NCLEX practice test, just look at the grid to see how well you are doing. Each grey square in the grid will turn green or red, depending if your answer to the question is right or wrong. With each question, the squares of the grid will turn green with your correct answers or red with the incorrect ones.
How are the practice tests arranged?
Each of our practice tests falls into one of the four NCLEX healthcare categories: Physiological Integrity, Safe and Effective Care Environment, Health Promotion and Maintenance, and Psychosocial Integrity. Each category includes practice tests that cover the subcategories. We also plan to offer tests that will take all the questions and split them into specific topics, such as pharmacology, laboratory tests, medical emergencies, etc.
Where do these questions come from?
These questions resemble those on the NCLEX. We designed them to simulate the real exam provided by the National Council of State Boards of Nursing (NCSBN). Many of the questions were created by our authors. Others were kindly provided by the Khan Academy under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 United States License.
What happens if I get a question wrong?
If the answer is correct, you will see a green checkmark and can go to the next question. It it’s wrong, you will see a red “x” and the correct answer. The rationale for the correct answer will also show, so you can read it and find out more. Taking notes on the questions you need to study will reinforce your learning.
Do I need to register to access the tests or the results?
No. You don't need an account to access our NCLEX practice tests or the results. We use a browser cookie to remember your progress so that you can safely close your browser window and come back at any time to the exact point at which you left off. No usernames or passwords to remember!
Is there a passing score for the practice tests?
We’ve set the passing score for the practice tests at 50%. The NCLEX-RN and NCLEX-PN are pass/fail examinations designed to determine if you have an entry-level knowledge of nursing. While we can’t promise that getting 50% or higher on the Nurse Plus practice test guarantees that you will pass your NCLEX, you'll have an indication of subjects that you know, as well as those that need more study.
Can I take a practice test more than once?
Absolutely! Our practice tests work the same way as flash cards. Each time you retake any of the tests, the questions and options will automatically shuffle into a different order. Random ordering is a proven learning method.
What if I don’t understand a question or agree with an answer?
We’re always glad to hear from Nurse Plus users. If a question can be improved or corrected, please let us know. Send us an email at [email protected]. We review all comments and respond to users as soon as possible.
NCLEX Tips and Tricks

Mometrix Test Preparation
Learn how to pass the NCLEX-RN exam and be prepared for your test day.

Nikole Bourgeois
How I Studied and PASSED NCLEX-RN with 5 EASY tips!
Monique and Monae
Learn how to pass NCLEX in 75 questions!
The Nurse Plus Academy is a part of Elegant E-Learning, Inc., a twelve-year-old company with a proven track record of revolutionizing online education. Our flagship site, Driving-Tests.org, is now in its twelfth year of operation as a trusted web presence for US learner drivers. It fills a niche in the driver education and driver safety marketplace by making free permit practice tests, written by experts, available to anyone who wants to study.
With Nurse Plus and CNA Plus, we're on a mission to help you pass your NCLEX and CNA tests. These sites provide practice tests that simulate the official exams provided by the National Council of State Boards of Nursing (NCSBN).
PNLE I Nursing Practice
Scope of this Nursing Test I is parallel to the NP1 NLE Coverage:
- Foundation of Nursing
- Nursing Research
- Professional Adjustment
- Leadership and Management
1. The registered nurse is planning to delegate tasks to unlicensed assistive personnel (UAP). Which of the following task could the registered nurse safely assigned to a UAP?
- Monitor the I&O of a comatose toddler client with salicylate poisoning
- Perform a complete bed bath on a 2-year-old with multiple injuries from a serious fall
- Check the IV of a preschooler with Kawasaki disease
- Give an outmeal bath to an infant with eczema
2. A nurse manager assigned a registered nurse from telemetry unit to the pediatrics unit. There were three patients assigned to the RN. Which of the following patients should not be assigned to the floated nurse?
- A 9-year-old child diagnosed with rheumatic fever
- A young infant after pyloromyotomy
- A 4-year-old with VSD following cardiac catheterization
- A 5-month-old with Kawasaki disease
3. A nurse in charge in the pediatric unit is absent. The nurse manager decided to assign the nurse in the obstetrics unit to the pediatrics unit. Which of the following patients could the nurse manager safely assign to the float nurse?
- A child who had multiple injuries from a serious vehicle accident
- A child diagnosed with Kawasaki disease and with cardiac complications
- A child who has had a nephrectomy for Wilm’s tumor
- A child receiving an IV chelating therapy for lead poisoning
4. The registered nurse is planning to delegate task to a certified nursing assistant. Which of the following clients should not be assigned to a CAN?
- A client diagnosed with diabetes and who has an infected toe
- A client who had a CVA in the past two months
- A client with Chronic renal failure
- A client with chronic venous insufficiency
5. The nurse in the medication unit passes the medications for all the clients on the nursing unit. The head nurse is making rounds with the physician and coordinates clients’ activities with other departments. The nurse assistant changes the bed lines and answers call lights. A second nurse is assigned for changing wound dressings; a licensed practitioner nurse takes vital signs and bathes theclients. This illustrates of what method of nursing care?
- Case management method
- Primary nursing method
- Team method
- Functional method
6. A registered nurse has been assigned to six clients on the 12-hour shift. The RN is responsible for every aspect of care such as formulating the care of plan, intervention and evaluating the care during her shift. At the end of her shift, the RN will pass this same task to the next RN in charge. This nursing care illustrates of what kind of method?
- primary nursing method
- case method
- team method
- functional method
7. A newly hired nurse on an adult medicine unit with 3 months experience was asked to float to pediatrics. The nurse hesitates to perform pediatric skills and receive an interesting assignment that feels overwhelming. The nurse should:
- resign on the spot from the nursing position and apply for a position that does not require floating
- Inform the nursing supervisor and the charge nurse on the pediatric floor about the nurse’s lack of skill and feelings of hesitations and request assistance
- Ask several other nurses how they feel about pediatrics and find someone else who is willing to accept the assignment
- Refuse the assignment and leave the unit requesting a vacation a day
8. An experienced nurse who voluntarily trained a less experienced nurse with the intention of enhancing the skills and knowledge and promoting professional advancement to the nurse is called a:
- team leader
- case manager
- change agent
9. The pediatrics unit is understaffed and the nurse manager informs the nurses in the obstetrics unit that she is going to assign one nurse to float in the pediatric units. Which statement by the designated float nurse may put her job at risk?
- “I do not get along with one of the nurses on the pediatrics unit”
- “I have a vacation day coming and would like to take that now”
- “I do not feel competent to go and work on that area”
- “ I am afraid I will get the most serious clients in the unit”
10. The newly hired staff nurse has been working on a medical unit for 3 weeks. The nurse manager has posted the team leader assignments for the following week. The new staff knows that a major responsibility of the team leader is to:
- Provide care to the most acutely ill client on the team
- Know the condition and needs of all the patients on the team
- Document the assessments completed by the team members
- Supervise direct care by nursing assistants
11. A 15-year-old girl just gave birth to a baby boy who needs emergency surgery. The nurse prepared the consent form and it should be signed by:
- The Physician
- The Registered Nurse caring for the client
- The 15-year-old mother of the baby boy
- The mother of the girl
12. A nurse caring to a client with Alzheimer’s disease overheard a family member say to the client, “if you pee one more time, I won’t give you any more food and drinks”. What initial action is best for the nurse to take?
- Take no action because it is the family member saying that to the client
- Talk to the family member and explain that what she/he has said is not appropriate for the client
- Give the family member the number for an Elder Abuse Hot line
- Document what the family member has said
13. Which is true about informed consent?
- A nurse may accept responsibility signing a consent form if the client is unable
- Obtaining consent is not the responsibility of the physician
- A physician will not subject himself to liability if he withholds any facts that are necessary to form the basis of an intelligent consent
- If the nurse witnesses a consent for surgery, the nurse is, in effect, indicating that the signature is that of the purported person and that the person’s condition is as indicated at the time of signing
14. A mother in labor told the nurse that she was expecting that her baby has no chance to survive and expects that the baby will be born dead. The mother accepts the fate of the baby and informs the nurse that when the baby is born and requires resuscitation, the mother refuses any treatment to her baby and expresses hostility toward the nurse while the pediatric team is taking care of the baby. The nurse is legally obligated to:
- Notify the pediatric team that the mother has refused resuscitation and any treatment for the baby and take the baby to the mother
- Get a court order making the baby a ward of the court
- Record the statement of the mother, notify the pediatric team, and observe carefully for signs of impaired bonding and neglect as a reasonable suspicion of child abuse
- Do nothing except record the mother’s statement in the medical record
15. The hospitalized client with a chronic cough is scheduled for bronchoscopy. The nurse is tasks to bring the informed consent document into the client’s room for a signature. The client asks the nurse for details of the procedure and demands an explanation why the process of informed consent is necessary. The nurse responds that informed consent means:
- The patient releases the physician from all responsibility for the procedure.
- The immediate family may make decision against the patient’s will.
- The physician must give the client or surrogates enough information to make health care judgments consistent with their values and goals.
- The patient agrees to a procedure ordered by the physician even if the client does not understand what the outcome will be.
16. A hospitalized client with severe necrotizing ulcer of the lower leg is schedule for an amputation. The client tells the nurse that he will not sign the consent form and he does not want any surgery or treatment because of religious beliefs about reincarnation. What is the role of the RN?
- call a family meeting
- discuss the religious beliefs with the physician
- encourage the client to have the surgery
- inform the client of other options
17. While in the hospital lobby, the RN overhears the three staff discussing the health condition of her client. What would be the appropriate nursing action for the RN to take?
- Tell them it is not appropriate to discuss the condition of the client
- Ignore them, because it is their right to discuss anything they want to
- Join in the conversation, giving them supportive input about the case of the client
- Report this incident to the nursing supervisor
18. A staff nurse has had a serious issue with her colleague. In this situation, it is best to:
- Discuss this with the supervisor
- Not discuss the issue with anyone. It will probably resolve itself
- Try to discuss with the colleague about the issue and resolve it when both are calmer
- Tell other members of the network what the team member did
19. The nurse is caring to a client who just gave birth to a healthy baby boy. The nurse may not disclose confidential information when:
- The nurse discusses the condition of the client in a clinical conference with other nurses
- The client asks the nurse to discuss the her condition with the family
- The father of a woman who just delivered a baby is on the phone to find out the sex of the baby
- A researcher from an institutionally approved research study reviews the medical record of a patient
20. A 17-year-old married client is scheduled for surgery. The nurse taking care of the client realizes that consent has not been signed after preoperative medications were given. What should the nurse do?
- Call the surgeon
- Ask the spouse to sign the consent
- Obtain a consent from the client as soon as possible
- Get a verbal consent from the parents of the client
21. A 12-year-old client is admitted to the hospital. The physician ordered Dilantin to the client. In administering IV phenytoin (Dilantin) to a child, the nurse would be most correct in mixing it with:
- Normal Saline
- Heparinized normal saline
- 5% dextrose in water
- Lactated Ringer’s solution
22. The nurse is caring to a client who is hypotensive. Following a large hematemesis, how should the nurse position the client?
- Feet and legs elevated 20 degrees, trunk horizontal, head on small pillow
- Low Fowler’s with knees gatched at 30 degrees
- Supine with the head turned to the left
- Bed sloped at a 45 degree angle with the head lowest and the legs highest
23. The client is brought to the emergency department after a serious accident. What would be the initial nursing action of the nurse to the client?
- assess the level of consciousness and circulation
- check respirations, circulation, neurological response
- align the spine, check pupils, check for hemorrhage
- check respiration, stabilize spine, check circulation
24. A nurse is assigned to care to a client with Parkinson’s disease. What interventions are important if the nurse wants to improve nutrition and promote effective swallowing of the client?
- Eat solid food
- Give liquids with meals
- Feed the client
- Sit in an upright position to eat
25. During tracheal suctioning, the nurse should implement safety measures. Which of the following should the nurse implements?
- limit suction pressure to 150-180 mmHg
- suction for 15-20 seconds
- wear eye goggles
- remove the inner cannula
26. The nurse is conducting a discharge instructions to a client diagnosed with diabetes. What sign of hypoglycemia should be taught to a client?
- warm, flushed skin
- hunger and thirst
- increase urinary output
- palpitation and weakness
27. A client admitted to the hospital and diagnosed with Addison’s disease. What would be the appropriate nursing action to the client?
- administering insulin-replacement therapy
- providing a low-sodium diet
- restricting fluids to 1500 ml/day
- reducing physical and emotional stress
28. The nurse is to perform tracheal suctioning. During tracheal suctioning, which nursing action is essential to prevent hypoxemia?
- aucultating the lungs to determine the baseline data to assess the effectiveness of suctioning
- removing oral and nasal secretions
- encouraging the patient to deep breathe and cough to facilitate removal of upper-airway secretions
- administering 100% oxygen to reduce the effects of airway obstruction during suctioning.
29. An infant is admitted and diagnosed with pneumonia and suspicious-looking red marks on the swollen face resembling a handprint. The nurse does further assessment to the client. How would the nurse document the finding?
- Facial edema with ecchymosis and handprint mark: crackles and wheezes
- Facial edema, with red marks; crackles in the lung
- Facial edema with ecchymosis that looks like a handprint
- Red bruise mark and ecchymosis on face
30. On the evening shift, the triage nurse evaluates several clients who were brought to the emergency department. Which in the following clients should receive highest priority?
- an elderly woman complaining of a loss of appetite and fatigue for the past week
- A football player limping and complaining of pain and swelling in the right ankle
- A 50-year-old man, diaphoretic and complaining of severe chest pain radiating to his jaw
- A mother with a 5-year-old boy who says her son has been complaining of nausea and vomited once since noon
31. A 80-year-old female client is brought to the emergency department by her caregiver, on the nurse’s assessment; the following are the manifestations of the client: anorexia, cachexia and multiple bruises. What would be the best nursing intervention?
- check the laboratory data for serum albumin, hematocrit, and hemoglobin
- talk to the client about the caregiver and support system
- complete a police report on elder abuse
- complete a gastrointestinal and neurological assessment
32. The night shift nurse is making rounds. When the nurse enters a client’s room, the client is on the floor next to the bed. What would be the initial action of the nurse?
- chart that the patient fell
- call the physician
- chart that the client was found on the floor next to the bed
- fill out an incident report
33. The nurse on the night shift is about to administer medication to a preschooler client and notes that the child has no ID bracelet. The best way for the nurse to identify the client is to ask:
- The adult visiting, “The child’s name is ____________________?”
- The child, “Is your name____________?”
- Another staff nurse to identify this child
- The other children in the room what the child’s name is
34. The nurse caring to a client has completed the assessment. Which of the following will be considered to be the most accurate charting of a lump felt in the right breast?
- “abnormally felt area in the right breast, drainage noted”
- “hard nodular mass in right breast nipple”
- “firm mass at five ‘ clock, outer quadrant, 1cm from right nipple’
- “mass in the right breast 4cmx1cm
35. The physician instructed the nurse that intravenous pyelogram will be done to the client. The client asks the nurse what is the purpose of the procedure. The appropriate nursing response is to:
- outline the kidney vasculature
- determine the size, shape, and placement of the kidneys
- test renal tubular function and the patency of the urinary tract
- measure renal blood flow
36. A client visits the clinic for screening of scoliosis. The nurse should ask the client to:
- bend all the way over and touch the toes
- stand up as straight and tall as possible
- bend over at a 90-degree angle from the waist
- bend over at a 45-degree angle from the waist
37. A client with tuberculosis is admitted in the hospital for 2 weeks. When a client’s family members come to visit, they would be adhering to respiratory isolation precautions when they:
- wash their hands when leaving
- put on gowns, gloves and masks
- avoid contact with the client’s roommate
- keep the client’s room door open
38. An infant is brought to the emergency department and diagnosed with pyloric stenosis. The parents of the client ask the nurse, “Why does my baby continue to vomit?” Which of the following would be the best nursing response of the nurse?
- “Your baby eats too rapidly and overfills the stomach, which causes vomiting
- “Your baby can’t empty the formula that is in the stomach into the bowel”
- “The vomiting is due to the nausea that accompanies pyloric stenosis”
- “Your baby needs to be burped more thoroughly after feeding”
39. A 70-year-old client with suspected tuberculosis is brought to the geriatric care facilities. An intradermal tuberculosis test is schedule to be done. The client asks the nurse what is the purpose of the test. Which of the following would be the best rationale for this?
- reactivation of an old tuberculosis infection
- increased incidence of new cases of tuberculosis in persons over 65 years old
- greater exposure to diverse health care workers
- respiratory problems are characteristic in this population
40. The nurse is making a health teaching to the parents of the client. In teaching parents how to measure the area of induration in response to a PPD test, the nurse would be most accurate in advising the parents to measure:
- both the areas that look red and feel raised
- The entire area that feels itchy to the child
- Only the area that looks reddened
- Only the area that feels raised
41. A community health nurse is schedule to do home visit. She visits to an elderly person living alone. Which of the following observation would be a concern?
- Picture windows
- Unwashed dishes in the sink
- Clear and shiny floors
- Brightly lit rooms
42. After a birth, the physician cut the cord of the baby, and before the baby is given to the mother, what would be the initial nursing action of the nurse?
- examine the infant for any observable abnormalities
- confirm identification of the infant and apply bracelet to mother and infant
- instill prophylactic medication in the infant’s eyes
- wrap the infant in a prewarmed blanket and cover the head
43. A 2-year-old client is admitted to the hospital with severe eczema lesions on the scalp, face, neck and arms. The client is scratching the affected areas. What would be the best nursing intervention to prevent the client from scratching the affected areas?
- elbow restraints to the arms
- Mittens to the hands
- Clove-hitch restraints to the hands
- A posey jacket to the torso
44. The parents of the hospitalized client ask the nurse how their baby might have gotten pyloric stenosis. The appropriate nursing response would be:
- There is no way to determine this preoperatively
- Their baby was born with this condition
- Their baby developed this condition during the first few weeks of life
- Their baby acquired it due to a formula allergy
45. A male client comes to the clinic for check-up. In doing a physical assessment, the nurse should report to the physician the most common symptom of gonorrhea, which is:
- pus in the urine
- WBC in the urine
46. Which of the following would be the most important goal in the nursing care of an infant client with eczema?
- preventing infection
- maintaining the comfort level
- providing for adequate nutrition
- decreasing the itching
47. The nurse is making a discharge instruction to a client receiving chemotherapy. The client is at risk for bone marrow depression. The nurse gives instructions to the client about how to prevent infection at home. Which of the following health teaching would be included?
- “Get a weekly WBC count”
- “Do not share a bathroom with children or pregnant woman”
- “Avoid contact with others while receiving chemotherapy”
- “Do frequent hand washing and maintain good hygiene”
48. The nurse is assigned to care the client with infectious disease. The best antimicrobial agent for the nurse to use in handwashing is:
- Isopropyl alcohol
- Hexachlorophene (Phisohex)
- Soap and water
- Chlorhexidine gluconate (CHG) (Hibiclens)
49. The mother of the client tells the nurse, “ I’m not going to have my baby get any immunization”. What would be the best nursing response to the mother?
- “You and I need to review your rationale for this decision”
- “Your baby will not be able to attend day care without immunizations”
- “Your decision can be viewed as a form of child abuse and neglect”
- “You are needlessly placing other people at risk for communicable diseases”
50. The nurse is teaching the client about breast self-examination. Which observation should the client be taught to recognize when doing the examination for detection of breast cancer?
- tender, movable lump
- pain on breast self-examination
- round, well-defined lump
- dimpling of the breast tissue
Answers and Rationales
- D. Bathing an infant with eczema can be safely delegated to an aide; this task is basic and can competently performed by an aid.
- B. The RN floated from the telemetry unit would be least prepared to care for a young infant who has just had GI surgery and requires a specific feeding regimen.
- C. RN floated from the obstetrics unit should be able to care for a client with major abdominal surgery, because this nurse has experienced caring for clients with cesarean births.
- A. The patient is experiencing a potentially serious complication related to diabetes and needs ongoing assessment by an RN
- D. It describes functional nursing. Staff is assigned to specific task rather than specific clients.
- B. Case management. The nurse assumes total responsibility for meeting the needs of the client during her entire duty.
- B. The nurse is ethically obligated to inform the person responsible for the assignment and the person responsible for the unit about the nurse’s skill level. The nurse therefore avoids a situation of abandoningclients and exposing them to greater risks
- A. This describes a mentor
- B. This action demonstrates a lack of responsibility and the nurse should attempt negotiation with the nurse manager.
- B. The team leader is responsible for the overall management of all clients and staff on the team, and this information is essential in order to accomplish this
- C. Even though the mother is a minor, she is legally able to sign consent for her own child.
- B. This response is the most direct and immediate. This is a case of potential need for advocacy and patient’s rights.
- D. The nurse who witness a consent for treatment or surgery is witnessing only that the client signed the form and that the client’s condition is as indicated at the time of signing. The nurse is not witnessing that the client is “informed”.
- C. Although the statements by the mother may not create a suspicion of neglect, when they are coupled with observations about impaired bonding and maternal attachment, they may impose the obligation to report child neglect. The nurse is further obligated to notify caregivers of refusal to consent to treatment
- C. It best explains what informed consent is and provides for legal rights of the patient
- B. The physician may not be aware of the role that religious beliefs play in making a decision about surgery.
- A. The behavior should be stopped. The first step is to remind the staff that confidentiality may be violated
- C. Waiting for emotions to dissipate and sitting down with the colleague is the first rule of conflict resolution.
- C. The nurse has no idea who the person is on the phone and therefore may not share the information even if the patient gives permission
- A. The priority is to let the surgeon know, who in turn may ask the husband to sign the consent.
- A. Phenytoin (Dilantin) can cause venous irritation due to its alkalinity, therefore it should be mixed with normal saline.
- A. This position increases venous return, improves cardiac volume, and promotes adequate ventilation and cerebral perfusion
- D. Checking the airway would be a priority, and a neck injury should be suspected
- D. Client with Parkinson’s disease are at a high risk for aspiration and undernutrition. Sitting upright promotes more effective swallowing.
- C. It is important to protect the RN’s eyes from the possible contamination of coughed-up secretions
- D. There has been too little food or too much insulin. Glucose levels can be markedly decreased (less than 50 mg/dl). Severe hypoglycemia may be fatal if not detected
- D. Because the client’s ability to react to stress is decreased, maintaining a quiet environment becomes a nursing priority. Dehydration is a common problem in Addison’s disease, so close observation of the client’s hydration level is crucial.
- D. Presuctioning and postsuctioning ventilation with 100% oxygen is important in reducing hypoxemia which occurs when the flow of gases in the airway is obstructed by the suctioning catheter.
- B. This is an example of objective data of both pulmonary status and direct observation on the skin by the nurse.
- C. These are likely signs of an acute myocardial infarction (MI). An acute MI is a cardiovascular emergency requiring immediate attention. Acute MI is potentially fatal if not treated immediately.
- D. Assessment and more data collection are needed. The client may have gastrointestinal or neurological problems that account for the symptoms. The anorexia could result from medications, poor dentition, or indigestion, and the bruises may be attributed to ataxia, frequent falls, vertigo or medication.
- B. This is closest to suggesting action-assessment, rather than paperwork- and is therefore the best of the four.
- C. The only acceptable way to identify a preschooler client is to have a parent or another staff member identify the client.
- C. It describes the mass in the greatest detail.
- C. Intravenous pyelogram tests both the function and patency of the kidneys. After the intravenous injection of a radiopaque contrast medium, the size, location, and patency of the kidneys can be observed by roentgenogram, as well as the patency of the urethra and bladder as the kidneys function to excrete the contrast medium.
- C. This is the recommended position for screening for scoliosis. It allows the nurse to inspect the alignment of the spine, as well as to compare both shoulders and both hips.
- A. Handwashing is the best method for reducing cross-contamination. Gowns and gloves are not always required when entering a client’s room.
- B. Pyloric stenosis is an anomaly of the upper gastrointestinal tract. The condition involves a thickening, or hypertrophy, of the pyloric sphincter located at the distal end of the stomach. This causes a mechanical intestinal obstruction, which leads to vomiting after feeding the infant. The vomiting associated with pyloric stenosis is described as being projectile in nature. This is due to the increasing amounts of formula the infant begins to consume coupled with the increasing thickening of the pyloric sphincter.
- B. Increased incidence of TB has been seen in the general population with a high incidence reported in hospitalized elderly clients. Immunosuppression and lack of classic manifestations because of the aging process are just two of the contributing factors of tuberculosis in the elderly.
- D. Parents should be taught to feel the area that is raised and measure only that.
- C. It is a safety hazard to have shiny floors because they can cause falls.
- D. The first priority, beside maintaining a newborn’s patent airway, is body temperature.
- B. The purpose of restraints for this child is to keep the child from scratching the affected areas. Mittens restraint would prevent scratching, while allowing the most movement permissible.
- C. Pyloric stenosis is not a congenital anatomical defect, but the precise etiology is unknown. It develops during the first few weeks of life.
- B. Pus is usually the first symptom, because the bacteria reproduce in the bladder.
- A. Preventing infection in the infant with eczema is the nurse’s most important goal. The infant with eczema is at high risk for infection due to numerous breaks in the skin’s integrity. Intact skin is always the infant’s first line of defense against infection.
- D. Frequent hand washing and good hygiene are the best means of preventing infection.
- D. CHG is a highly effective antimicrobial ingredient, especially when it is used consistently over time.
- A. The mother may have many reasons for such a decision. It is the nurse’s responsibility to review this decision with the mother and clarify any misconceptions regarding immunizations that may exist.
- D. The tumor infiltrates nearby tissue, it can cause retraction of the overlying skin and create a dimpling appearance.
Related Posts
PNLE : Maternal and Child Health Nursing Exam 2
PNLE III for Medical Surgical Nursing
PNLE: FON Practice Exam for Infection, Asepsis, Basic concept of Stress and Illness
NCLEX Practice Questions Test Bank for Free
Ready to conquer the NCLEX- RN exam and launch your nursing career? You’ve come to the right place!
Welcome to our ultimate 2024 NCLEX guide—a treasure trove of over 1,000 free practice questions crafted to boost your confidence and sharpen your skills. But that’s just the beginning! Dive deep into:
- A comprehensive primer on the NCLEX-RN exam to familiarize yourself with the test format.
- Answers to the most frequently asked questions about the NCLEX.
- An in-depth look at question types you’ll encounter.
- A detailed overview of the NCLEX-RN test plan .
- Expert test-taking tips and strategies to give you that extra edge.
Let’s embark on this journey together and turn your nursing dreams into reality!
Table of Contents
Nclex-rn practice questions test bank, what is nclex.
- What is Next Generation NCLEX (NGN)?
Safe and Effective Care Environment
- Health Promotion and Maintenance
- Psychosocial Integrity
Physiological Integrity
Clinical judgment, integrated processes, item writers for nclex, computer adaptive test (cat), 95% confidence interval rule, maximum-length exam, run-out-of-time (r.o.o.t.) rule, zero/one (0/1) scoring, plus/minus (+/-) scoring, rationale scoring, pretest items, testing time, unfolding case study, stand-alone items, multiple response select all that apply.
- Multiple Response Select N
Multiple Response Grouping
- Highlight in Text
Highlight in Table
Matrix multiple response, matrix multiple choice.
- Drag and Drop Cloze
Drag and Drop Rationale
Drop down cloze, drop down rationale, drop down in table, chart or exhibit questions, graphic option, select all that apply or multiple-response, fill-in-the-blank, ordered-response, how to register for the nclex, nclex-rn resources, want more practice questions, recommended resources.
Looking for the complete collection of practice questions? For more NCLEX practice questions, please visit our Nursing Test Bank here .
We have included more than 1,000+ NCLEX practice questions covering different nursing topics for this nursing test bank ! We’ve made a significant effort to provide you with the most challenging questions along with insightful rationales for each question to reinforce learning .
We recommend you do all practice questions before you take the actual exam. Doing so will help reduce your test anxiety and help identify nursing topics you need to review. To make the most of the practice exams, try to minimize mistakes to less than 15 questions and take your time answering the questions, especially when reading the rationales.
Quiz Guidelines
Before you start, here are some examination guidelines and reminders you must read:
- Practice Exams : Engage with our Practice Exams to hone your skills in a supportive, low-pressure environment. These exams provide immediate feedback and explanations, helping you grasp core concepts, identify improvement areas, and build confidence in your knowledge and abilities.
- You’re given 2 minutes per item.
- For Challenge Exams, click on the “Start Quiz” button to start the quiz.
- Complete the quiz : Ensure that you answer the entire quiz. Only after you’ve answered every item will the score and rationales be shown.
- Learn from the rationales : After each quiz, click on the “View Questions” button to understand the explanation for each answer.
- Free access : Guess what? Our test banks are 100% FREE. Skip the hassle – no sign-ups or registrations here. A sincere promise from Nurseslabs: we have not and won’t ever request your credit card details or personal info for our practice questions. We’re dedicated to keeping this service accessible and cost-free, especially for our amazing students and nurses. So, take the leap and elevate your career hassle-free!
- Share your thoughts : We’d love your feedback, scores, and questions! Please share them in the comments below.
Included NCLEX-RN question sets for this nursing test bank are as follows. Please click on the links below and you’ll be redirected to the quiz page:
NEW UPDATE: Introducing Challenge Exams and Practice Exams
Engage with these new modes to enhance your learning journey, each tailored to meet different needs and propel you towards academic achievement.
- Dive into Practice Exam Mode for a supportive learning experience. Here, real-time feedback aids in understanding core concepts and building confidence. It’s your space for growth and preparation.
- Step up to Challenge Exam Mode to test your mastery. With rigorous questions, a leaderboard, and a timer, it’s designed to assess your readiness and foster a competitive spirit.
Test your mastery with these Challenge Exams :
Build your confidence and grasp core concepts with these Practice Exams :
The National Council Licensing Examination (NCLEX) is a comprehensive test administered by the National Council of State Boards of Nursing (NCSBN). It assesses whether candidates possess the necessary knowledge and skills to provide safe and effective nursing care at the entry level. The NCLEX is available in two versions: the NCLEX-RN for registered nurses and the NCLEX-PN for practical/vocational nurses.
The NCSBN, composed of nursing regulatory bodies from all 50 states in the US, the District of Columbia, and four US territories, is responsible for safeguarding the public by ensuring safe nursing care. It sets the standards and guidelines for nursing licensure and develops the NCLEX examinations.
Becoming a registered nurse (RN) requires meeting specific licensure requirements determined by the licensing authorities in each jurisdiction governed by the NCSBN. One of these requirements is passing the NCLEX-RN, which evaluates the competencies necessary for practicing safely and effectively as an entry-level RN. The NCLEX-RN is used by member boards of nursing and many Canadian nursing regulatory bodies to inform their licensure decisions.
What is Next Generation NCLEX (NGN)?
The Next Generation NCLEX (NGN) is currently in effect this April 2023 for RN and LPN / LVN candidates. The change in the NCLEX is driven by the need to adapt to the increasing complexity of client care, advancements in healthcare practice, and the demand for safe clinical decision-making . The NGN aims to address the declining ability of new nursing graduates to make safe clinical decisions by integrating clinical judgment as a key competency. The NGN test format will remain adaptive but with fewer test items. Candidates will encounter Unfolding Case Studies and Stand-Alone Items , scored using partial credit with three different scoring rules. These changes in the NGN aim to assess critical thinking and the ability to make safe clinical judgments during various phases of client care.
In summary, the following are the key changes between the previous NCLEX format and the Next Generation NCLEX (NGN):
- Same adaptive test format but reduced number of items. The Next Generation NCLEX (NGN) will retain the adaptive test format, similar to the current NCLEX, but with fewer test items. Candidates will answer between 85 and 150 items, with 15 as pretest or unscored items.
- Case studies. All candidates will encounter three (3) Unfolding Case Studies, each consisting of six test items (a total of 18 items). Clinical situation information will be presented to candidates in a medical record format resembling a table-like structure. These situations are designed to assess their ability to think critically and make safe clinical decisions across different phases of client care. In addition to the case studies, some candidates may have Stand-Alone Items for their NGN exam.
- New NGN item types. The NGN exam will feature new item types, which include questions in unfolding cases and stand-alone items, highlight, cloze, matrix, bow-tie, drag and drop, and extended multiple responses.
- Scoring differences. NGN test items will be scored differently compared to the current NCLEX. They will utilize partial credit scoring with three different scoring rules: the 0/1 scoring rule, the +/- scoring rule, and the rationale scoring rule. These are explained further below.
NCLEX-RN Test Plan
The NCLEX test plan is a content guideline to determine the distribution of test questions. NCSBN uses the “Client Needs” categories to ensure the NCLEX covers a full spectrum of nursing activities. It is a summary of the content and scope of the NCLEX to serve as a guide for candidates preparing for the exam and to direct item writers in the development of items. Additionally, to assess the knowledge, skills, abilities, and clinical judgment necessary for entry-level nursing practice , the NCLEX-RN Test Plan utilizes Bloom’s taxonomy for the cognitive domain. This taxonomy provides a foundation for writing and coding examination items, focusing on application-level or higher-level cognitive abilities that require advanced thought processing.
The content of the NCLEX-RN is organized into four major Client Needs categories: Safe and Effective Care Environment, Health Promotion and Maintenance, Psychosocial Integrity, and Physiological Integrity. Some of these categories are divided further into subcategories. Below is the NCLEX-RN test plan effective as of April 2023 until March 2026:
There are two subcategories under Safe and Effective Care Environment.
- Management of Care category includes content that tests the nurse ‘s knowledge and ability to direct nursing care that enhances the care delivery setting to protect clients, significant others, and healthcare personnel.
- Safety and Infection Control category includes content that tests the nurse’s ability required to protect clients, families, and healthcare personnel from health and environmental hazards.
Health Promotion and Maintenance
Health Promotion and Maintenance category includes content that tests the nurse’s ability to provide and direct nursing care to the client that incorporates knowledge of expected growth and development, preventing and early detection of health problems, and strategies to achieve optimal health.
Psychosocial Integrity
The Psychosocial Integrity category is content related to the promotion and support for the emotional, mental, and social well-being of the client experiencing stressful events and clients with acute or chronic mental illness .
In the Physiological Integrity category are items that test the nurse’s ability to promote physical health and wellness by providing care and comfort , reducing risk potential, and managing health alterations. There are four subcategories under Physiological Integrity.
- Basic Care and Comfort are content to test the nurse’s ability to provide comfort and assistance to the client in performing activities of daily living .
- Pharmacological and Parenteral Therapies category includes content to test the nurse’s ability to administer medications and parenteral therapies ( IV therapy , blood administration, and blood products).
- Reduction of Risk Potential category includes content to test the nurse’s ability to prevent complications or health problems related to the client’s condition or prescribed treatments or procedures.
- Physiological Adaptation category includes questions that test the nurse’s ability to provide care to clients with acute, chronic, or life-threatening conditions.
Clinical judgment is a central component of the NCLEX-RN Test Plan, reflecting the evolving demands and complexity of nursing practice . Nurses must engage in an iterative, multi-step process that utilizes nursing knowledge to observe and assess situations, identify client concerns, and generate evidence-based solutions to ensure safe client care. Clinical judgment questions are represented through Unfolding Case Studies or individual Stand-Alone Items , with case studies addressing each step of clinical judgment. The following are the six clinical judgment cognitive skills:
- Recognize cues “What matters most?” Identifying relevant and important information from various sources, such as medical history , laboratory studies, and vital signs.
- Analyze cues “What could it mean?” Organizing and connecting recognized cues to the client’s clinical presentation.
- Prioritize hypotheses “Where do I start?” Evaluating and prioritizing hypotheses based on urgency, likelihood, risk, difficulty, time constraints, and other factors.
- Generate solutions “What can I do?” Identifying expected outcomes and using hypotheses to define a set of interventions aligned with the expected outcomes.
- Take action “What will I do?” Implementing the highest-priority solution(s) identified.
- Evaluate outcomes “Did it help?” Comparing observed outcomes to expected outcomes to assess the effectiveness of interventions.
Additionally, In contrast to the nursing process or ADPIE , the NCSBN focuses on AAPIE ( assessment , analysis, planning , intervention, evaluation ), wherein nursing diagnosis is not tested at the current NGN because it is not considered a universal language used in health care or the nursing profession. In nursing practice and for the NGN, students must use their pathophysiology knowledge to analyze client assessments and connect them with common conditions in healthcare settings.
Integral to nursing practice, several processes are integrated throughout the Client Needs categories and subcategories:
- Caring. In an atmosphere of mutual respect and trust, nurses interact with clients, providing encouragement, hope, support, and compassion to help achieve desired outcomes .
- Clinical Judgment . An observed outcome of critical thinking and decision-making , clinical judgment (discussed above) is a dynamic and iterative process. It involves using nursing knowledge to observe and assess situations, prioritize client concerns, generate evidence-based solutions, and deliver safe client care.
- Communication and Documentation . Verbal and nonverbal interactions between nurses, clients, significant others, and the healthcare team. Accurate and comprehensive documentation ensures adherence to practice standards and accountability in care provision.
- Culture and Spirituality. Recognizing and considering the unique preferences, standards of care, and legal considerations of clients (individuals, families, groups, and populations) in the context of their culture and spirituality.
- Nursing Process. A systematic approach to client care encompassing assessment , analysis, planning, implementation , and evaluation .
- Teaching/Learning. Facilitating acquiring knowledge, skills, and abilities that promote behavioral change.
Who writes questions for the NCLEX? The NCSBN sets the criteria and selection process for item writers who are registered nurses. Many of them are nursing educators with an advanced degrees in nursing, so if you’ve completed an accredited nursing program, you have already taken several tests written by nurses with backgrounds similar to those who write for the NCLEX.
The NCLEX-RN is a crucial step for registered nurse (RN) candidates seeking licensure. Administered through computerized adaptive testing ( CAT ), this examination utilizes computer technology and measurement theory to create a personalized and accurate assessment of each candidate’s knowledge and skills.
The CAT system employed in the NCLEX-RN ensures that each candidate receives a unique examination tailored to their abilities. As the test progresses, the computer selects items from a large item pool based on the candidate’s previous answers. These items are classified according to the test plan categories, difficulty levels, and clinical judgment steps. The CAT system continually recalculates the candidate’s ability estimate and selects subsequent items accordingly, creating an exam that aligns with the NCLEX-RN Test Plan requirements. This dynamic approach allows candidates to demonstrate their competence effectively.
Additionally, unlike traditional fixed-length exams, which assign the same items to all candidates, CAT selects items based on the candidate’s ability, resulting in a more accurate assessment. The CAT scoring algorithm estimates the candidate’s ability by considering all previous answers and the difficulty level of those items. By administering items that challenge the candidate appropriately, the exam gathers maximum information about their ability.
Pass or Fail Decisions: How to Pass the NCLEX?
Passing the NCLEX-RN requires you, the candidate, to meet a specific passing standard established by the NCSBN Board of Directors (BOD). The passing standard represents the minimum ability level necessary for safe and effective entry-level nursing practice. The BOD reevaluates this standard every three years, considering various factors such as a standard-setting exercise conducted by experts and psychometricians, historical data on candidate performance, and information on the educational readiness of aspiring nurses. Once the passing standard is set, it is uniformly applied to all candidates during the scoring process. The NCSBN indicates that these three rules govern pass-or-fail decisions: the 95% Confidence Interval Rule , Maximum-Length Exam Rule , and Run-Out-Of-Time Rule .
In this scenario, the computer stops administering test questions when it is 95% certain that your ability is clearly above the passing standard or clearly below the passing standard.
When your ability is close to the passing standard, the CAT gives you items until the maximum number of items is reached. At this point, the computer disregards the 95% confidence rule and decides whether you pass or fail by your final ability estimate. If your final ability estimate is above the passing standard, you pass; if it is below, you fail.
In the event that a candidate runs out of time before completing the maximum number of items and the computer has not reached a 95% certainty regarding the candidate’s pass or fail status, alternative criteria come into play.
- If the candidate has not answered the minimum required number of items, the candidate will automatically fail.
- If the candidate has answered at least the minimum required number of items, the final ability estimate will be determined based on all the responses given before the exam time expires. If the score meets or exceeds the passing standard, the candidate will pass. Otherwise, the candidate will fail.
New Scoring System in the Next Generation NCLEX
The Next Generation NCLEX (NGN) incorporates different item formats, and for items that have multiple correct answers, partial credit scoring is implemented . Unlike the previous exam format, where items are scored as either all correct or all incorrect, the NGN will use polytomous scoring models to evaluate partial understanding. For example, in the previous version of NCLEX (multiple response) SATA (select-all-that-apply) items, only endorsing all the correct options results in a correct score. However, the new approach will acknowledge partial understanding, allowing differentiation between candidates with different numbers of correct options. This change will provide a more accurate assessment of candidates’ knowledge, skills, and abilities.
Three methods are used to assign partial credit for these items: plus/minus scoring, zero/one scoring, and rationale scoring. Understanding the scoring models is crucial for NCLEX-RN takers to know how their answers are evaluated and how scores are determined.
The 0/1 scoring rule is used for multiple-choice items. Choosing the correct option earns one point while selecting an incorrect option gives a score of zero. This rule applies to single response items, including the example multiple-choice item.
The +/– scoring rule measures a candidate’s ability to identify relevant information. It assigns points for correct options and deducts points for incorrect options. It is used for multi-point items, and the total score is calculated by adding correct options and subtracting incorrect ones. The lowest possible score is zero. This rule is applied to NGN question types such as multiple-response and select all that apply.
The rationale scoring rule is used for questions that assess paired information. To earn a score of one point, both answer options must be correct. If either option is incorrect, the score is 0.
How Many Questions Are on the NCLEX?
All RN candidates must answer a minimum of 85 items , while a maximum of 150 items be administered during the five-hour time allotment. Each NCLEX-RN exam includes 15 pretest items (unscored), which are indistinguishable from operational (scored) items.
To ensure the effectiveness of computerized adaptive testing (CAT) in the NCLEX, the difficulty level of each item needs to be determined beforehand. This is achieved by administering these items as pretest items to a large group of NCLEX candidates. Since the difficulty of pretest items is initially unknown, they are not part of your score and are not considered when evaluating a candidate’s ability or determining pass-fail outcomes. Once a sufficient number of responses are collected, the pretest items undergo statistical analysis and calibration. If they meet the required NCLEX statistical standards, they can be used as operational items in future exams. Therefore, candidates must approach every item with their best effort, regardless of whether it is a pretest or an operational item.
The length of the NCLEX-RN examination varies for each candidate based on their responses, but there is a five-hour time limit for the exam, including all breaks. To ensure completion within the allotted time, candidates must maintain a reasonable pace, spending approximately one to two minutes per item . It’s important to note that the length of the examination does not determine pass or fail outcomes; candidates can succeed or fail regardless of the examination’s duration.
Case Studies in NGN
The Next Generation NCLEX (NGN) has introduced case studies that present practical clinical scenarios and include test items aligned with six cognitive abilities of the clinical judgment model. The scenario can occur in various settings, and the client’s outcome can vary, including improvement, stability, or decline with complications. Laboratory results, if included, are presented in a table, and abnormal values are highlighted with an “L” or “H”. There are two types of case studies: Unfolding Case Study with six test items assessing specific skills and Stand-Alone Items with a single test item independent of a case study.
An Unfolding Case Study presents a realistic client situation with evolving data resembling a medical record. It includes multiple phases over time, reflecting changes in the client’s condition. The case study evaluates all six cognitive skills of the clinical judgment model through six questions. Each test-taker receives three (3) unfolding case studies, totaling 18 items across those cases.
Stand-Alone Items are case studies with a single question, with the item presented as a bow-tie or a trend question type. Candidates who take more than the minimum number of items on the NCLEX receive around six to seven stand-alone cases.
Question Types in the NCLEX-RN
The different question types for the NCLEX-RN include the following:
Extended Multiple Response
In Extended Multiple Response item types, test-takers can choose one or more options in Multiple Response Select All That Apply, select a specific number of items in Multiple Response Select N, or choose options from different groupings presented in a table in Multiple Response Grouping, with scoring rules based on the selected type. Extended multiple response may include the following formats:
The Multiple Response Select All That Apply item type allows test-takers to choose one or more answer options. It uses the +/- Scoring Rule, where selecting correct information earns points (+1), and selecting incorrect information results in points deducted (-1). The maximum points achievable are equal to the number of correct options, and the minimum score is 0, with no negative scores. The item must have a minimum of five options and can have up to ten options, with the possibility of all ten options being correct.
Multiple Response Select N
The Multiple Response Select N item type informs the test-taker about the specific number of items (N) that can be selected. The question provides a range of options, with a minimum of five and a maximum of ten options. It uses the 0/1 Scoring Rule, where each correct response earns 1 point, while any incorrect response results in 0 points.
The Multiple Response Grouping utilizes a table to present options, with a minimum of two and a maximum of five groupings. Each grouping consists of a minimum of two and a maximum of four options, ensuring an equal number of options within each grouping. Test-takers are required to select at least one option from each grouping. The item follows the +/- Scoring Rule, meaning there is no negative score per grouping. The total score for the item is determined by summing the points earned within each grouping. The maximum score achievable equals the number of keys (N).
For this NGN item type, the test-taker is presented with information and must highlight specific parts of the information provided. Highlight question type include the following formats:
Highlight in Text
It involves a paragraph of information where the test-taker must select (highlight) specific parts of the text based on the question’s requirements. The item can include a maximum of ten options for selection and uses the +/- Scoring Rule.
The Highlight in Table item type involves a table of information. The candidate is tasked with selecting (highlighting) specific parts of the text within the table based on the question’s prompt. The item can include a maximum of ten options for selection. The table has two columns, including a header, and can have up to five rows. This item type uses the +/- Scoring Rule.
Matrix/Grid
In the Matrix NGN item type, test-takers are presented with a grid-like structure to which they must respond. There are two variations: Matrix Multiple Response, where each column can have multiple correct responses, and Matrix Multiple Choice, where test-takers select one answer option per row. Extended multiple response may include the following formats:
The Matrix Multiple Response item type consists of response columns, where each column can have multiple correct responses. The item can have between two and ten columns and four to seven rows. In each column, at least one response option must be selected, but it is possible to select one or more responses per column. The item follows the +/- Scoring Rule, with no negative score per column. The total score for the item is determined by summing the points earned within each column. The maximum score achievable is equal to the number of keys (N).
The item includes a minimum of four rows and a maximum of ten rows. It can have either two or three options/columns. Test-takers are allowed to select one answer option per row. The item follows the 0/1 scoring rule, where the test-taker earns 1 point for each correct response and 0 points for incorrect responses. The total score for the item is obtained by summing the scores over the rows. The maximum score achievable is equal to the number of rows.
Drag and Drop
In the Drag and Drop NGN question type, test-takers are presented with options to drag and drop into specific targets. There are two variations: Drag and Drop Cloze, where options are placed in response targets to complete sentences and Drag and Drop Rationale, where options are matched to causes and effects. Drag and drop may include the following formats:
Drag and Drop Cloze
The Drag and Drop Cloze item type includes a range of four to ten options. It can have one or more response targets where the options are dragged to. The item must have a minimum of one sentence with one target per sentence and up to five sentences, each with one target per sentence. The item follows the 0/1 Scoring Rule, where a correct response earns 1 point and incorrect responses earn 0 points. The total score is obtained by summing the scores across all targets, with the maximum score achievable being the number of targets.
The Drag and Drop Rationale type involves one sentence with one cause and one effect or one sentence with one cause and two effects. The sentence can be a single dyad (one sentence with two targets) or a single triad (one sentence with three targets). Each drag & drop target can have three to five options. The item follows the Rationale Scoring Rule where both answer options must be correct to earn a point.
The Drop Down question type in NGN includes three variations: Drop Down Cloze, Drop Down Rationale, and Drop Down in Table. Drop down may include the following formats:
The Drop Down Cloze item type presents one or two sentences of information that require completion using drop-down options. Each drop-down can contain three to five options. The item must have a minimum of one sentence with one drop-down per sentence and can include up to five sentences, each with one drop-down. The item follows the 0/1 Scoring Rule, where the score is calculated by summing the correct responses across all drop-downs. The maximum score achievable is equal to the number of drop-downs.
The Drop Down Rationale item type presents either one sentence with one cause and one effect or one sentence with one cause and two effects. Each drop-down can contain three to five options. The scoring follows the Rationale Scoring Rule, where X and Y must be correct to earn one point. The maximum points that can be earned are 1 point for a dyad (one sentence with two targets) and 2 points for a triad (one sentence with three targets).
The Drop Down in Table item type presents a table of information with drop-down options located in various parts of the table. The item must have a minimum of three columns and three rows and a maximum of five columns and four rows. One column serves as the header column. Each row contains one drop-down. The item follows the 0/1 Scoring Rule, where the score is calculated by summing the correct responses across all drop-downs. The maximum score achievable is equal to the number of drop-downs.
The Bow-tie item type is visually designed to resemble a bow-tie shape. It consists of five options on the left side, five options on the right side, and four options in the middle well of the bow-tie. The item addresses all of the cognitive skills within a single item. The Bow-tie item follows the 0/1 scoring rule. The left and right wells have two answer options each, while the middle well has one answer option, resulting in a maximum possible score of 5 points. Each correct response earns 1 point, while incorrect responses earn 0 points.
The Trend item type presents information in a medical record or flow sheet format that spans over time, requiring the test-taker to analyze information across different points in time. The item addresses multiple cognitive skills within a single item. It can utilize any NGN item type except for the bow-tie. The scoring rule for the Trend item depends on the specific item type used.
Multiple-Choice Questions
Many questions on the NCLEX are in multiple-choice format. This traditional text-based question will provide you data about the client’s situation, and you can only select one correct answer from the given four options. Multiple-choice questions may vary and include: audio clips, graphics, exhibits, or charts.

A chart or exhibit is presented along with a problem. You’ll be provided with three tabs or buttons that you need to click to obtain the information needed to answer the question. Select the correct choice among four multiple-choice answer options.
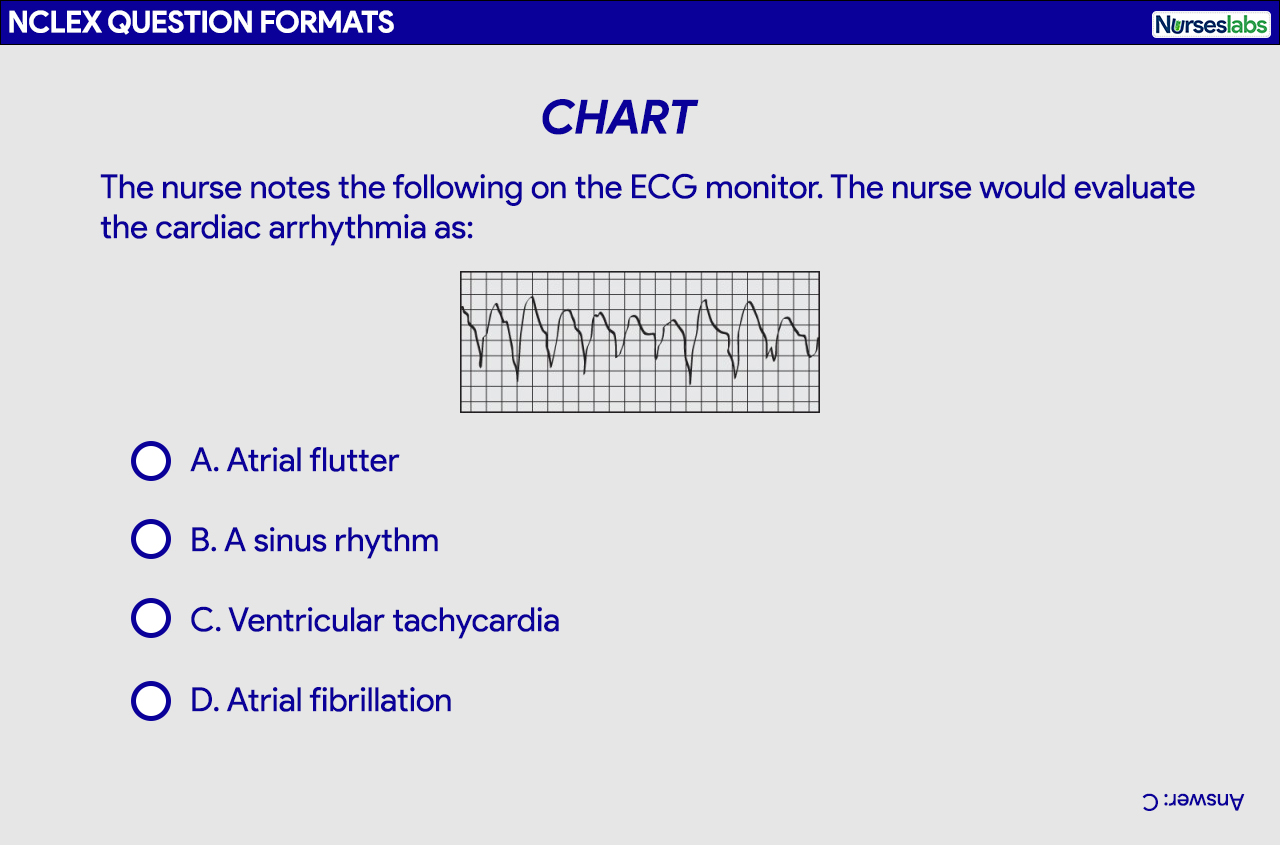
In this format, four multiple-choice answer options are pictures rather than text. Each option is preceded by a circle that you need to click to represent your answer.
In an audio question format, you’ll be required to listen to a sound to answer the question. You’ll need to use the headset provided and click on the sound icon for it to play. You’ll be able to listen to the sound as many times as necessary. Choose the correct choice from among four multiple-choice answer options.
For the video question format, you must view an animation or a video clip to answer the following question. Select the correct choice among four multiple-choice answer options.
Multiple-response or select all that apply (SATA) alternate format question requires you to choose all correct answer options that relate to the information asked by the question. There are usually more than four possible answer options. No partial credit is given in scoring these items (i.e., selecting only 3 out of the 5 correct choices), so you must select all correct answers for the item to be counted as correct.
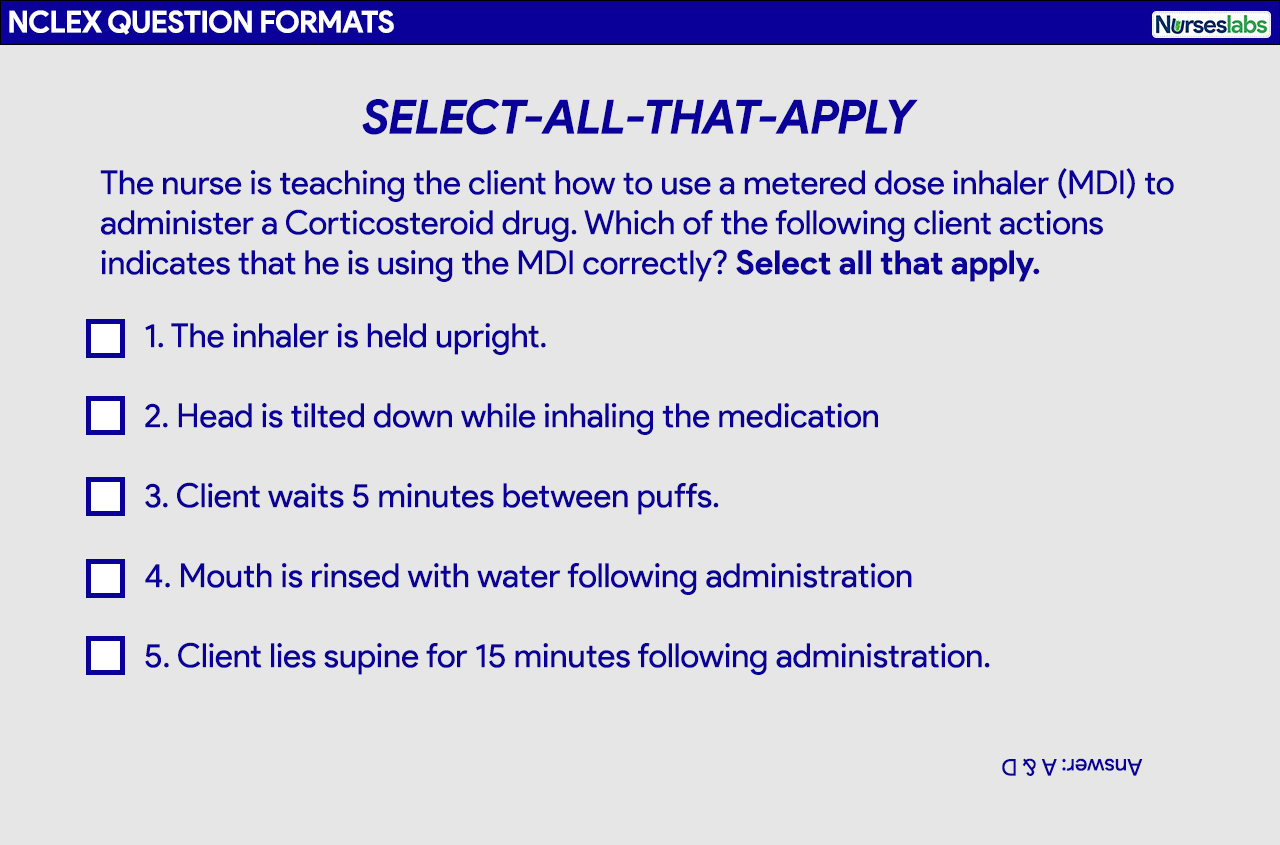
Tips when answering Select All That Apply Questions
- You’ll know it’s a multiple-response or SATA question because you’ll explicitly be instructed to “Select all that apply.”
- Treat each answer choice as a True or False by rewording the question and proceed to answer each option by responding with a “yes” or “no”. Go down the list of answer options one by one and ask yourself if it’s a correct answer.
- Consider each choice as a possible answer separate to other choices. Never group or assume they are linked together.
The fill-in-the-blank question format is usually used for medication calculation, IV flow rate calculation, or determining the intake-output of a client. You’ll be asked to perform a calculation in this question format and type in your answer in the blank space provided.
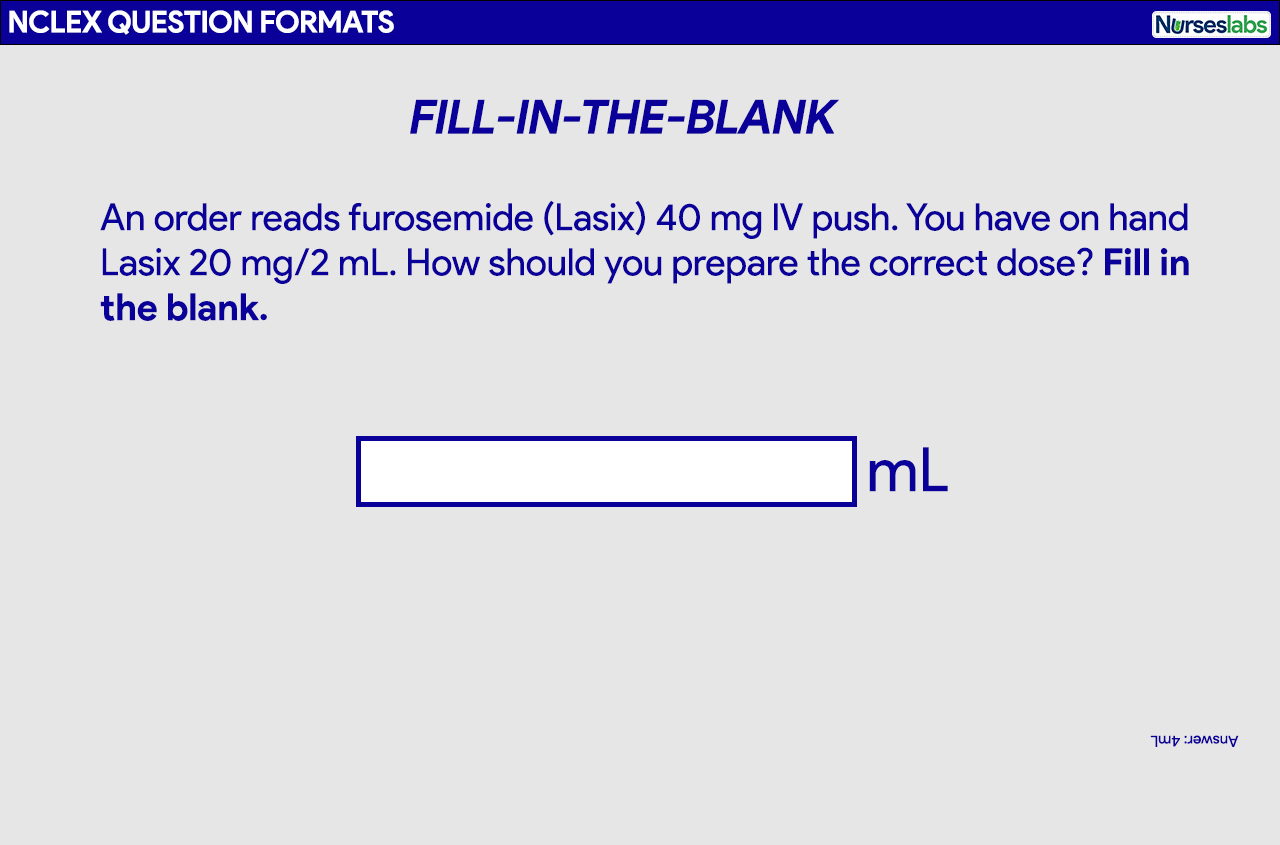
Tips when answering Fill-in-the-Blank
- Always follow the specific directions as noted on the screen.
- There will be an on-screen calculator on the computer for you to use.
- Do not put any words, units of measurements, commas, or spaces with your answer, type only the number. Only the number goes into the box.
- Rounding an answer should be done at the end of the calculation or as what the question specified, and if necessary, type in the decimal point.
In an ordered-response question format, you’ll be asked to use the computer mouse to drag and drop your nursing actions in order or priority. Based on the information presented, determine what you’ll do first, second, third, and so forth. Directions are provided with the question.

Tips when answering Ordered-Response questions
- Questions are usually about nursing procedures. Imagine yourself performing the procedure to help you answer these questions.
- You’ll have to place the options in correct order by clicking an option and dragging it on the box on the right. You can rearrange them before you hit submit for your final answer.
A picture or graphic will be presented along with a question. This could contain a chart, a table, or an illustration where you’ll be asked to point or click on a specific area. Figures may also appear along with a multiple-choice question. Be as precise as possible when marking the location.
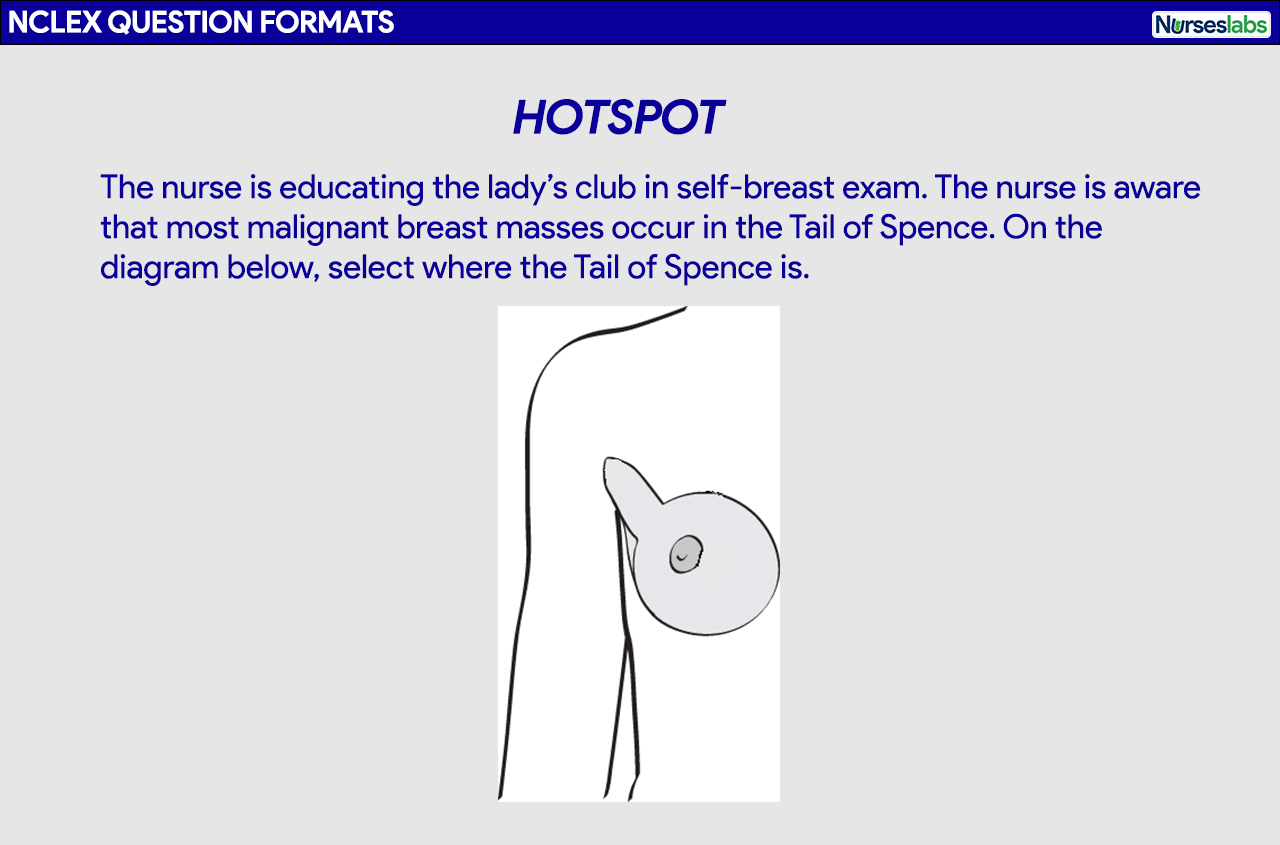
Tips when answering Hotspot questions
- Mostly used to evaluate your knowledge of anatomy, physiology, and pathophysiology.
- Locate anatomical landmarks to help you select the location needed by the item.
So you’ve finally decided to take the NCLEX, the next step is registration or application for the exam. The following are the steps on how to register for the NCLEX, including some tips:
- Application to the Nursing Regulatory Board (NRB). The initial step in the registration process is to submit your application to the state board of nursing in the state in which you intend to obtain licensure. Inquire with your board of nursing regarding the specific registration process as requirements may vary from state to state.
- Registration with Pearson VUE. Once you have received the confirmation from the board of nursing that you have met all of their state requirements, proceed, register, and pay the fee to take the NCLEX with Pearson VUE . Follow the registration instructions and complete the forms precisely and accurately.
- Authorization to Test. If you were made eligible by the licensure board, you will receive an Authorization to Test (ATT) form from Pearson VUE. You must test within the validity dates (an average of 90 days) on the ATT. There are no extensions or you’ll have to register and pay the fee again. Your ATT contains critical information like your test authorization number, validity date, and candidate identification number.
- Schedule your Exam Appointment. The next step is to schedule a testing date, time, and location at Pearson VUE. The NCLEX will take place at a testing center , you can make an exam appointment online or by telephone. You will receive a confirmation via email of your appointment with the date and time you choose including the directions to the testing center. * Changing Your Exam Appointment. You can change your appointment to test via Pearson VUE or by calling the candidate services. Rules for scheduling , rescheduling, and unscheduling are explained further here . Failing to arrive for the examination or failure to cancel your appointment to test without providing notice will forfeit your examination fee and you’ll have to register and pay again.
- On Exam Day. Arrive at the testing center on your exam appointment date at least 30 minutes before the schedule. You must have your ATT and acceptable identification (driver’s license, passport, etc) that is valid, not expired, and contains your photo and signature.
- Processing Results. You will receive your official results from the board of nursing after six weeks.
Important list and resources you need to know if you’re taking the NCLEX:
- 2023 NCLEX Candidate Bulletin. This resource is a comprehensive guide for the NCLEX, providing essential information and contact details for candidates. It covers registration procedures, test fees, scheduling , testing accommodations, exam rules, and what to bring to the test site. The guide also includes details on the check-in process, breaks, technical issues, and the testing environment. It explains the results reporting process and retake-policy and provides information on the content, development, and test plans of the NCLEX. Additionally, it discusses the passing standard, item formats, and decision rules for passing or failing the exam.
- Sample Questions and Exam Preview. Get a headstart on your exam preparation with these sample test packs by the NCSBN.
- Candidate Tutorial. With the new item types, we highly recommend testing how the Next Generation NCLEX (NGN) works. This tutorial guides you on interacting with different question types in your NCLEX exam. It provides a representative sample of items you may encounter during the test, allowing you to practice their functionality.
Please visit our Nursing Test Bank page if you’re looking to answer more practice questions from different topics and different question formats.
Recommended books and resources for your NCLEX success:
Disclosure: Included below are affiliate links from Amazon at no additional cost from you. We may earn a small commission from your purchase. For more information, check out our privacy policy .
Saunders Comprehensive Review for the NCLEX-RN Saunders Comprehensive Review for the NCLEX-RN Examination is often referred to as the best nursing exam review book ever. More than 5,700 practice questions are available in the text. Detailed test-taking strategies are provided for each question, with hints for analyzing and uncovering the correct answer option.

Strategies for Student Success on the Next Generation NCLEX® (NGN) Test Items Next Generation NCLEX®-style practice questions of all types are illustrated through stand-alone case studies and unfolding case studies. NCSBN Clinical Judgment Measurement Model (NCJMM) is included throughout with case scenarios that integrate the six clinical judgment cognitive skills.

Saunders Q & A Review for the NCLEX-RN® Examination This edition contains over 6,000 practice questions with each question containing a test-taking strategy and justifications for correct and incorrect answers to enhance review. Questions are organized according to the most recent NCLEX-RN test blueprint Client Needs and Integrated Processes. Questions are written at higher cognitive levels (applying, analyzing, synthesizing, evaluating, and creating) than those on the test itself.

NCLEX-RN Prep Plus by Kaplan The NCLEX-RN Prep Plus from Kaplan employs expert critical thinking techniques and targeted sample questions. This edition identifies seven types of NGN questions and explains in detail how to approach and answer each type. In addition, it provides 10 critical thinking pathways for analyzing exam questions.

Illustrated Study Guide for the NCLEX-RN® Exam The 10th edition of the Illustrated Study Guide for the NCLEX-RN Exam, 10th Edition. This study guide gives you a robust, visual, less-intimidating way to remember key facts. 2,500 review questions are now included on the Evolve companion website. 25 additional illustrations and mnemonics make the book more appealing than ever.

NCLEX RN Examination Prep Flashcards (2023 Edition) NCLEX RN Exam Review FlashCards Study Guide with Practice Test Questions [Full-Color Cards] from Test Prep Books. These flashcards are ready for use, allowing you to begin studying immediately. Each flash card is color-coded for easy subject identification.

191 thoughts on “NCLEX Practice Questions Test Bank for Free”
How much are you charging for it?
Thanks for being generous
Thank you for your kindness & generosity. This is a big help for us, especially those with financial constraints.
How much for this
Thanks Matt Vera for your utmost effort in helping nurses to pass the exam
You’re most welcome! Good luck on your exams!
Hello Matt do you still have the Test Bank questions for 2021. If you do can I have them please and thank you.
Hi Winnie, Please visit our
Thanks heaps! Matt..
The site is very useful.
Thank you mam/sir
This is very helpful site. god bless🤗
Great website wish l knew about it before taking my nclex
Thank you so much for this free site. I found it just as helpful as Kaplan and Sanders which I paid for. I recommended this nurseslabs to some of my nurse friends preparing for the NCLEX. I used it to study and passed my NCLEX October 28. I will continue to use this as a reference. Once again Thank-You. A.Haynes RN
Hey Matt, I am impressed by your generosity. I couldn’t believe these were all free. In all fairness, there should be a tab for donations for the constant upkeep of the web. A very minimal way to show our gratitude.
Although I just started nursing school the i formation is mind blowing and very useful for me already. Thank you for your generosity. I will be using all the practice quizzes and test to prepare myself. Thank you again.
Thank you for this free nclex practice tests! May you have more blessings and success! I will take my exam next month.
Very informative and helpful
Thank you!You’re a big blessing to those who will take the exam.
I can’t thank you enough for this gift you have given us to use . God bless you.
Thank you so much Matt! This is helping me work toward my NCLEX with less pressure.
Thanks a lot can I get reading materials on PDF please
Thanks Matt Vera for ingenious effort.
You are heaven sent, Thank you Matt for helping us.
you guys all thank you so much for this massively hard work and huge success for all the nurses around the world .
Your efforts are immeasurable, you are not only helping nurses to pass their NCLEX exams but also increasing the number of qualified/competent nurses providing healthcare around the globe. We are grateful. I used this site to prepare for internal exams whilst I was in school and it really helped me. I’ll be writing NCLEX soon..
Planning to start this process, I think this will be so helpful to me. Thankyou very much
Thank you so much Nurse matt vera for this qbank,most beneficial, God bless you., if I may ask for some videos or pictures associated with the questions, will also help e.g lung sounds,abdominal sound etc thank you
I loved your blog and thanks for publishing this about NCLEX practice questions!! I am really happy to come across this exceptionally well written content. Thanks for sharing and look for more in future!! Keep doing this inspirational work and share with us.
My name is Daniel m Johnson from Tanzania I’m holding diploma in nursing and midwifery I’m looking for different nurse from different country so as we can share ideas and experience since I’m student I need to no much thing about nursing ….any one who is touched to please help me I wish to be came a good nurse and help different people from different society
What a wonderful thing to do for people! Thank you very much.
This very helpful to me, thank you.
You did a great job Matt…
This is so lovely
Very useful site. Thank you so much.
This is an amazing job Matt!! REALLY INCREDIBLE!!!
With all this I will certainly pass my NCLEX exams.
THANK YOU so so much Matt, this is great beyond measure.. I have been hook to this website. God will bless you and yours abundantly
You’re most welcome! :)
i just want to confirm for #39 it state pt need additional teaching so E should also be included to the answer cause it was contraindicated to MS right? . thank you :)
Yes, this has been corrected. Thank you! :)
Very informative and helpful. Thank you so much Sir/ madam
Thank you for providing regarding NCLEX preparation
Very informative. Thank you for update.
This is for sure the best nurse’s website ever. It really helped me a lot during my training.
Number 58 of NCLEX test 5 does not have the answers listed.
Hi Rebekah, this is now fixed. Thank you for letting us know!
This is very helpful
It’s very informative. Thanks
Thank you Matt Vera for providing information free of charge
Any advice of how well you can do on these question to build up your confidence?
Thanks a lot for great job. May the Lord Almighty shower His blessing upon you.
Thank you, this site is amazing. God bless you
Thanks alot.I,ve got a question What score ranges would be considered a Pass? I scored 69.33% overall. is that a Pass???
75% and above, from the analysis I got from a test after getting below 75
Thank you Nurse Matt. You deserve all the blessings! 🙏🏻😊
This is very helpful. Thank you Nurse Matt
Question 16 on practice test 9 asked about assessment during L sided CHF, yet the correct answer pertained to right sided HF. Just wanted to let you know…. Thanks for the practice questions! Appreciate all the work put into this.
Question 41 of NCLEX-RN Test 2 has two C choices. Thanks.
Hi, I like your questions, they’re very nice and challenging. Learning a lot from them.
I love this site.. Now all friends are learning serious from here
Thanks you guys are very generous
From Kenya, this site is so helpful,am learning a lot here.Thank you especially for the care plans.
Thank you so much
You Matt and your staff are such a blessing to us who will be taking the NCLEX RN exam. This site is very useful and helpful because it is very comprehensive and easy to understand. God bless and may tribe increase. Thank you so much
The site is very informative. I have learned a lot. Test questions are really amazing which I cannot find with other website. However, I got a low score, thus I need to further study especially on the areas wherein I got a below passing grade. I hope you will allow me. Thank you
thank you so much for creating this site for people like us. This excellent job. May God bless you in Jesus name —Amen
The Practice tests are awesome! The rationales are all well-explained which I love because it gives me more knowledge and insight. Thank you for creating this website free of charge.
Thank you so much. It was really helpful. I passed the exam. God bless real good.
Thank you Matt for the awesome and great website! its beyond compare. I want more practice test questions to hone my knowledge in Nursing practice, however, when I am trying to open one of the practice tests, I cant go through it. Could you please allow me? God bless
Thank you Matt for this practice test. Now I know my strength and weaknesses and will concentrate of the system that needs for further study. Can I practice more in practice test no 2? Please allow me to go trough with it. Kudos to you and your staff.
Hi this is what i got, im so nervous due to my nclex exam its gonna be this coming oct. Its doesnt say pass or not.
Your score 48% Categories Basic Care and Comfort 100% Health Promotion and Maintenance 53.85% Pharmacological and Parenteral Therapies 26.67% Physiological Adaptation 54.55% Psychosocial Integrity 100% Reduction of Risk Potential 36.36% Safety and Infection Control 100%
Thanks so much for this useful information. God bless you.
Thank you so much for all you do
The Practice tests are excellent. The rationales are all well-explained which I love because it gives me more knowledge and insight. Thank you for creating this website free of us. Remain blessed.
Like I am obsess with nurselab. A handy powerful tool, to keep you updated, thick and richly packed. You guys made reading so interesting and magnetic and very easy. Please do not stop. I recommend this to all nurses.
Love this. Thank you for sharing your generosity. I’ve been using this since I was still in college and I continue to use it until now.
Thank you so very much for this
I remain speechless but mostly grateful for your unconditional helpful assistance for this awesome richly throughout profound tool and opportunity given to me to increase my confidence, strengthen my knowledge, and be ready for my upcoming exam. Your questions and rationales are beyond my expectations. You are a God’ sent angel. Thank You. God Bless you. I will be forever grateful to you for making my dream come true! 🙌
This website can help me to review for NCLEX and it is for free! Thank you so much!
Amazing and really awesome job to you Matt and your entire team, may God replenish your source for giving us this for free. I have recommended to all my friends and family. Remain blessed and stay safe.
That’s very kind of you. Thank you so much! Bless you!
Your test questions have greatly helped me pass my NCLEX. I passed my NCLEX today and thank you to Nurseslabs. I came across this website by accident and I do not know how but it was divine intervention. I will definitely recommend Nurseslabs to my friends. The quality of the questions and rationales were very good and you would not think this is all for free the kind of work that came with it.
Kudos Nurseslabs and wishing all the future test takers all the best!
Wow Sam, congrats! What materials did you use other than nurseslabs? I’ve been answering nurseslabs also. My exam is on June. I hope I could also make it.
Thank you for this NCLEX sample test,as tool to determine areas i need to review/focus on for the proper exams.
This website can help me to review for NCLEX Thank you so much!
I just wanna ask why is that there are no more rationale posted after answering the question unlike before. Thanks by the way for the free and great Q & A bank. ❤
Sorry, we’re currently having some performance issues with that setup. Until we can resolve it, we have set each quiz to show results and rationales only after you have finished all the questions. Thank you for your understanding.
Hello, how do I get my score after taking the test to know if I am doing well or not
Hi, after you’re done answering all questions, the final item will direct you to the “Quiz Summary,” from there, click on the “Finish Quiz” button to get your final score.
Very great tool to study for the NCLEX. I passed my exam just by focusing on the questions and rationales provided here.
That’s great! Congratulations!
Thank you so much. It’s very helpful. God bless you…
Thank you for being generous. This is a big help.
I got 55/75.
Thank you so much for making this site.
Very helpful. Thank you and God bless…
Thank you so much, Nurse Matt for your generosity. Helping your fellow nurses and aspiring nurses to work abroad is such a selfless and noble act. God bless you and your team!
Thank you for your kind words, JB! Will pass on this message to the team. :) God bless!
The rationale after the question will really help us a lot specially when you are just using the question via online.
Hi Romel, we have temporarily changed this setting so that results and rationales will show only after you’ve finished the quiz. This is because we’re having some performance issues when using the previous setting. We’ll revert the changes once we’re sure the problem is resolved. Thanks for understanding!
I didn’t get my results after answering the 75 questions. Please why?
Hi Esther, did you click on the “Finish Quiz” button?
Thanks for all these questions where/how can i check my answers to these questions?
After answering the last item of the quiz, you’ll be redirected to the quiz summary. From there, click on the “Finish Quiz” button to view your score and results. You can also click on the “View Questions” button to review your answers and read the rationales.
Hi, thanks for providing so much useful information and all the test banks!
In RN practice Quiz 1:75 questions, for question 70, wonder if the correct phrase would be “would you NOT expect”?
Hi Cecilia, thanks for letting us know. We have corrected the question. Thank you! 🥰
Thank you for allowing me to practice the nurseslabs questions. The rationales are well explained. Thank you!
Thank you Ruth. Hope you’ve learned a lot from our practice questions. 🥰
God bless you
My name is Samuel. I just started with the RN practice questions. Thank you for the opportunity.
Hi, thank you so much for your generosity. Using this to prepare for my NCLEX and find it very informative. I will keep you posted on how it goes on the D-day
Frequently throughout the quiz, ARDS is given as “Adult Respiratory Distress Syndrome” instead of “Acute Respiratory Distress Syndrome”. This needs to be corrected.
Hi Bella, thanks for bringing this up.
Technically both terms are correct since “adult respiratory distress syndrome” is an earlier name referred to “acute respiratory distress syndrome” to differentiate it from respiratory distress syndrome in neonates and children. For the sake of uniformity, we have edited them to “acute respiratory distress syndrome”. You can read more about it here: https://doi.org/10.1164/ajrccm.149.3.7509706
This is so kind a gesture, remain blessed .The information is very understandable and helpful
I just wanted to thank you for taking the time to generate this website, this is really helpful and is free. God bless you
Thank you for your support and guide toward my nclex preparation.
Thanks for your generosity. I hope to pass my NCCLEX just on the first attempt Grateful for all your help
thanks for the help
Hi Sir, kindly explain why this question – The client with hyperemesis gravidarum is at risk for developing: Metabolic Acidosis is the answer. Thank you.
Quite familiar with the content. Thanks for this selfless initiative.
It has been a nice experience.
I love these practical questions. So helpful.
Thanks very much this is a good help for all students
Thank you for mett this free test which i have passed yesterday afternoon so ,it is greatest pleasure which will help me
Thank you so much for this great initiative.
Thanks for being kind God bless you
thank you for your help and kindness. It’s difficult to go back to school after 22 years of practice as a RN to take the test where you must cover a vast knowledge, which you do not use in everyday working (depends on the special field you are working. so I really appreciate your effort and dedication.
Matt Vera and all those helping us through this free medium, May God richly bless you abundantly. And may all your good desires come through
Hello Vera, I would start by thanking you for the great job you’ve done by helping us in our preparation for the exams. secondly would wish to know wther you have audio clips for lung, heart and abdominal sounds. thank you in advance and if any kindly let mh know pls.
What should we be scoring on these practice questions to let us know that we’re ready for the NCLEX
Do you have LPN test also?
Hi, please visit NCLEX-PN Practice Questions & Test Bank (200 Questions)
Thank you so much Nurse Matt you just don’t know how nurseslabs helped me in my nursing career and i even recommended nurseslabs to some of my friends. God bless you😊
Hi Matt, Thank you for this, indeed very helpful practice questions. Just a query though it says here to limit wrong answers to 15 or less? So is that the passing mark ? about 75-80%
Yes, that is correct. :)
Thank you so much for the practice questions. I learned a lot and it helped me to understand why I was getting my answers wrong. I used Kaplan and Saunders but it wasn’t helping me. I feel more confident than ever to retake my boards.
thank you…. wish this help a lot to my daughter to passed please pray for her God bless!!!
hi Matt, can l still use these question banks to study for the new NGN questions
Hi nurse Matt, May I gave all the questions please, need to prepare study for exam after been off school over 30 years, realize it for not giving up not try again, thank you 🙏
Thank you so much Nurselabs! I passed my NCLEX-RN exam using only your practice 75 question per day questions bank. I have a tight budget and not able to purchased online review and I just focused in answering your practice questions in just 2 weeks!!! Thank you for helping nurses! God Bless you more!
I want to practices questions
Hello Thanks so much for your good heart and good wish for us to practice and pass the NCLEX. Well appreciated. Please after your update I can’t get the answers and rationale to the 75 questions. This will help me to know my ability and where am lagging behind. Please how can this be rectified Thanks Hope
Hi Hope, did you finished all of the questions for the quiz? Your score together with the correct answers and rationale will only show after you’ve completed the whole quiz.
Hello Vera I finished all 75 questions submitted but no answer or rationale came up. I tried upto 3 times same. Even my friend I shared your content with complained of same thing, answers not coming. Please what can we do to access the answers and rationale Thanks Hope
What particular quiz?
Hello, great resource! I am a nurse that wants to help student nurses reach their full potential as nurses and pass the nclex. I would like to utilize your tests and quizzes to help my students learn to critically think through the questions and learn how to put their nursing knowledge to use. Would you allow me to utilize your questions in my content?
Thank you for the kind words! It’s awesome to hear that you’re dedicated to helping student nurses thrive. 🌟
Absolutely, you’re more than welcome to utilize our tests and quizzes for your students! We believe in collaborative efforts to strengthen the nursing community. Just ensure to give appropriate credit when using the content.
Out of curiosity, are there specific areas or topics you find students struggle with the most when preparing for the NCLEX? Maybe we can work together to create even more targeted resources!
Best of luck with your mission to guide the next generation of nurses!
Hi, I am studying for med surg 1 and med surg 2 upcoming exam. Need to pass both exams.
Sounds like you’ve got a busy study schedule ahead! MedSurg can be challenging, but with the right resources and dedication, you’ve got this. If you need specific materials, tips, or just a morale boost, don’t hesitate to reach out. Else, you can do practice all MedSurg exams on our Nursing Test Banks . Rooting for you to ace both exams! 💪
thank you so much… a big help
Hi Glacier and what a nice name!
You’re welcome! Really glad to hear the NCLEX practice questions were a big help. If you’ve got any other areas you’re prepping for or need more practice with, just let me know. Here to support your journey!
Thanks a lot @nurseslabs for this initiative I really believe by the time I sit my exam I will be a great nurse than ever before. I am learning a lot from the questions and explanation.
Hey Charles, You’re very welcome! I’m thrilled to hear that you’re finding our initiative helpful in your journey to becoming a great nurse. Remember, continuous learning is a key part of nursing practice, and it’s fantastic to see your dedication to it. If you ever come across any challenging topics or have questions about specific nursing concepts, please don’t hesitate to reach out. We’re here to support you every step of the way. Keep up the excellent work, and you’ll do great on your exam! 📖🏥🌟
Much help for beginners like us
Thank you so much Nurseslabs, I made it!!! Your practice exams, especially the rationales helped me a LOT…thank you!!!
Wow, that’s awesome news! 🌟 Huge congrats on making it through – your hard work and dedication really paid off. It’s super cool to hear how our practice exams and rationales played a part in getting you across the finish line.
Remember, this is just the beginning of an amazing journey in nursing. The field’s always changing and growing, and so will you. Keep that enthusiasm and curiosity going strong!
If you ever need a hand or just want to share your journey as you dive into your nursing career, give us a shout. We’re always here to cheer you on and lend support.
Big congrats again and best of luck out there!
Thanks for the information
thanks for the guide
Thank you for your kindness.
Thank you very much!
Thanks a lot for this whole range of knowledge; it’s now upon me to work extra hard to be a better nurse outside there or help other nurses be better at service delivery.
Hi Evans, You’re so welcome! I’m glad to hear that the range of knowledge from the NCLEX practice questions is empowering you to aim for excellence in nursing. Remember, every bit of effort counts towards becoming not just a better nurse but also a great mentor to others in the field. If you need more resources or advice along the way, I’m here to help. Keep up the fantastic work!
Please how can I practice questions please 🙏
In practice exam 5 question 22 asks about hyperemesis…. wouldn’t that cause alkalosis (rather than acidosis), since its acid from the stomach that is leaving the body?
Can I. Have free practice questions? NGN questions?
Thank you for the opportunity to know about all the information posted here. I strongly believe I will pass the NCLEX-RN exam at my first attempt through these useful resources available here. Thanks
Thanks a lot Nurselabs for the free test banks! It’s all what I focused to practice and read every rationale in each questions given. I just recently took my NCLEX-RN exam last week and i was able to make it. Your website is what i embraced and felt much comfortable and trusted what is in there. Thanks for helping lots of NURSES! Highly recommended!
Hello Brenda, Congratulations on passing your NCLEX-RN exam! 🎉 That’s a fantastic achievement, and I’m so thrilled to hear that our test banks and rationales were a valuable part of your preparation. Thank you for trusting Nurseslabs and for your kind words—it means a lot to us.
If you have any tips for future test-takers or any other resources you found particularly helpful, we’d love to hear about them. Your feedback not only celebrates your success but also helps us continue to improve and assist other nursing students.
Thanks again for recommending us, and best of luck in your exciting nursing career!
THIS IS GREAT. THANK YOU FOR SHARING.
Hello, Thank you for your good work. Are you uploading new practice tests or comprehensive tests for nclex rn or nclex pn soon? It has been a while.
Hi Monica, Thank you for your kind words! We appreciate your support. Yes, we are planning to upload new practice tests and comprehensive tests for both NCLEX RN and NCLEX PN very soon. Stay tuned for updates!
thanks for update ..be blessed
You’re doing great!!!! Thanks
Good day sir, please am Thomas from ghana and I want an assistance to enable me pass NCLEX test.
THANK YOU VERY MUCH.
Please can you help me with questions on surgery
Good day sir
hi i get only 50 to 60 % in all test is it good or bad
A female client is receiving I/ V Mannitol . An assessment specific to safe administration of the said drug is : A . Vitals signs q 4 h B. Weighing daily C. Urine output D. Level of consciousness q 4 h Please tell me the right answer ?? I’m comfusing here between option b and c because someone told me that if we gives diuretics ( mannitol) to pt then we asess weight daily , but many Students give answer C .. so I’m confusing here plz tell me the right answer??
Well explained answers thanks
Learn more and more question
Leave a Comment Cancel reply
Free NCLEX Questions
Looking for free NCLEX questions? We have hundreds of free questions for your test prep and review. These are challenging NCLEX practice questions with instant scoring. All of our questions include detailed explanations so that you can learn from your mistakes. These review questions will help you prepare for either the NCLEX-RN or the NCLEX-PN. Our practice tests have 75 questions each, and they cover all of the topics. To focus on a specific topic, choose from the category listing. Start your test prep right now with our free NCLEX questions!
NCLEX Practice Tests
NCLEX Practice Test 1
NCLEX Practice Test 2
NCLEX Practice Test 3
NCLEX Questions by Category
Management of Care
Safety & Infections
Health Promotion
Psychosocial Integrity
Basic Care & Comfort
Pharmacology
Risk Reduction
Physiological Adaptation
The National Council Licensure Examination is more commonly known as the NCLEX exam. This test is for the licensing of nurses in the U.S. and Canada, and it is taken after graduating from nursing school. There are two different versions of this nursing exam, the NCLEX-PN and the NCLEX-RN.
You will take the NCLEX-RN to obtain your registered nursing license, which is also known as the RN License. The NCLEX-PN is for the licensing of vocational or practical nurses, also known as the LPN license.
The tests are in the CAT format, which stands for Computerized Adaptive Testing. This type of test adapts to your abilities, asking more difficult questions as you get correct answers. This type of testing measures your ability more quickly, with fewer questions. It also reduces the advantage of guessing. The CAT format also allows more types of questions. In addition to regular multiple choice they also have alternate item formats. These include ordered response, fill-in-the-blank calculations, hot spots, and multiple response.
The NCLEX-RN has between 75 and 265 questions. If you are doing extremely well or extremely poorly, the test will stop after 75 questions, and you will be given your score. At most, you may have to answer up to 265 questions, as the computer works to evaluate your overall abilities and knowledge. The time limit is 6 hours. The NCLEX-PN has between 85 and 205 questions. The time limit for this exam is 5 hours.
These are both very challenging exams, so you will want to spend a lot of time on your test prep and review. One of the best ways to prepare is with NCLEX practice questions. You should work through these questions very carefully and study the explanations when you get a wrong answer. Get started right now with our free NCLEX questions!


IMAGES
VIDEO
COMMENTS
PNLE FON Practice Exam for Nursing Process, Physical and Health Assessment and Routine Procedures. 100 items. PNLE: FON Practice Exam for Oxygenation and Nutrition. 100 items. PNLE: Fundamentals in Nursing Exam 1. 25 items. PNLE: Fundamentals in Nursing Exam 2. 25 items. PNLE: Fundamentals in Nursing Exam 3.
These categories, or sections, and the percentage of questions you should expect to see in this examination are: Safe and Effective Care Environment. Coordinated Care (16% to 22%) Safety and Infection Control (10% to16%) Health Promotion and Maintenance (7% to 13%) Psychosocial Integrity (8% to 14%) Physiological Integrity.
Physiological Integrity: Physiological Adaptation. The NCLEX-RN Test Plan is organized into four major Client Needs categories. Two of the four categories are divided into subcategories as shown below: Safe and Effective Care Environment. Management of Care – 17% to 23%. Safety and Infection Control – 9% to 15%.
This NCLEX-PN practice test includes questions about Alzheimer’s Disease and dementia, mental health terms and situations, and therapeutic interventions by the nurse. Topics covered in this NCLEX-PN practice test include therapeutic responses to major life events, different types of abuse, and mental health terms.
Don’t waste time practicing low-level questions! Challenge yourself with our NCLEX-RN sample questions. Q1. Q2. Q3. Q4. Q5. The nurse is caring for a client at 39 weeks gestation who is receiving an IV oxytocin infusion for induction of labor. The nurse notes recurrent late decelerations on the fetal monitor.
The physician instructed the nurse that intravenous pyelogram will be done to the client. The client asks the nurse what is the purpose of the procedure. The appropriate nursing response is to: outline the kidney vasculature. determine the size, shape, and placement of the kidneys.
questions you can answer is 75 and a maximum of 265. Read the question and answers carefully—do not jump into conclusions or make wild guesses. Look for keywords—Avoid answers with absolutes like always, never, all, every, only, must, except, none, or no. Don’t read into the question—Never assume anything that has not been
Welcome to our ultimate 2024 NCLEX guide—a treasure trove of over 1,000 free practice questions crafted to boost your confidence and sharpen your skills. But that’s just the beginning! Dive deep into: A comprehensive primer on the NCLEX-RN exam to familiarize yourself with the test format.
DISCLAIMER:The site aways check and verify questions and answers however it is possible that we missed some thing. We recommend the user to always use other sources to verify or fact check information. If the user found some errors we are very happy to know, you can report such errors in our fb page or at [email protected].
The NCLEX-RN has between 75 and 265 questions. If you are doing extremely well or extremely poorly, the test will stop after 75 questions, and you will be given your score. At most, you may have to answer up to 265 questions, as the computer works to evaluate your overall abilities and knowledge. The time limit is 6 hours.