An official website of the United States government
Official websites use .gov A .gov website belongs to an official government organization in the United States.
Secure .gov websites use HTTPS A lock ( Lock Locked padlock icon ) or https:// means you've safely connected to the .gov website. Share sensitive information only on official, secure websites.
- Publications
- Account settings
- Advanced Search
- Journal List


Nurses’ Adherence to Patient Safety Principles: A Systematic Review
Mojtaba vaismoradi, susanna tella, patricia a logan, jayden khakurel, flores vizcaya-moreno.
- Author information
- Article notes
- Copyright and License information
Correspondence: [email protected] ; Tel.: +47-75517813
Received 2020 Feb 23; Accepted 2020 Mar 16; Issue date 2020 Mar.
Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license ( http://creativecommons.org/licenses/by/4.0/ ).
Background: Quality-of-care improvement and prevention of practice errors is dependent on nurses’ adherence to the principles of patient safety. Aims: This paper aims to provide a systematic review of the international literature, to synthesise knowledge and explore factors that influence nurses’ adherence to patient-safety principles. Methods: Electronic databases in English, Norwegian, and Finnish languages were searched, using appropriate keywords to retrieve empirical articles published from 2010–2019. Using the theoretical domains of the Vincent’s framework for analysing risk and safety in clinical practice, we synthesized our findings according to ‘patient’, ‘healthcare provider’, ‘task’, ‘work environment’, and ‘organisation and management’. Findings: Six articles were found that focused on adherence to patient-safety principles during clinical nursing interventions. They focused on the management of peripheral venous catheters, surgical hand rubbing instructions, double-checking policies of medicines management, nursing handover between wards, cardiac monitoring and surveillance, and care-associated infection precautions. Patients’ participation, healthcare providers’ knowledge and attitudes, collaboration by nurses, appropriate equipment and electronic systems, education and regular feedback, and standardization of the care process influenced nurses’ adherence to patient-safety principles. Conclusions: The revelation of individual and systemic factors has implications for nursing care practice, as both influence adherence to patient-safety principles. More studies using qualitative and quantitative methods are required to enhance our knowledge of measures needed to improve nurse’ adherence to patient-safety principles and their effects on patient-safety outcomes.
Keywords: adherence, quality of care, patient-safety principles, nursing intervention, practice errors, safe care
1. Introduction
The World Health Organization defines patient safety as the absence of preventable harm to patients and prevention of unnecessary harm by healthcare professionals [ 1 ]. It has been reported that unsafe care is responsible for the loss of 64 million disability-adjusted life years each year across the globe. Patient harm during the provision of healthcare is recognized as one of the top 10 causes of disability and death in the world [ 2 ]. Regarding the financial consequence of patient harm, a retrospective analysis of inpatient harm based on data collected from 24 hospitals in the USA showed that harm-reduction strategies could reduce total healthcare costs by $108 million U.S. and generate a saving of 60,000 inpatient care days [ 3 ]. Additionally, the loss of income and productivity due to other associated costs of patient harm are estimated to be trillions of dollars annually [ 4 ]. The burden of practice errors on patients, their family members, and the healthcare system can be reduced through implementing patient-safety principles based on preventive and quality-improvement strategies [ 5 ]. Patient-safety principles are scientific methods for achieving a reliable healthcare system that minimizes the incidence rate and impact of adverse events and maximizes recovery from such incidents [ 6 ]. These principles can be categorized as risk management, infection control, medicines management, safe environment and equipment [ 7 ], patient education and participation in own care, prevention of pressure ulcers, nutrition improvement [ 8 ], leadership, teamwork, knowledge development through research [ 9 ], feeling of responsibility and accountability, and reporting practice errors [ 10 ].
The nurses’ role is to preserve patient safety and prevent harm during the provision of care in both short-term and long-term care settings [ 11 , 12 ]. Nurses are expected to adhere to organizational strategies for identifying harms and risks through assessing the patient, planning for care, monitoring and surveillance activities, double-checking, offering assistance, and communicating with other healthcare providers [ 13 , 14 ]. In addition to clear policies, leadership, research driven safety initiatives, training of healthcare staff, and patient participation [ 1 , 15 ], nurses’ adherence to the principles of patient safety [ 16 , 17 ] is required for the success of interventions aimed at the prevention of practice errors and to achieve sustainable and safer healthcare systems.
Adherence to and compliance with guidelines and recommendations are influenced by personal willingness, culture, economic and social conditions, and levels of knowledge [ 18 , 19 ]. On the other hand, lack of adherence and compliance contravenes professional beliefs, norms, and expectations of the healthcare professional’s role [ 20 ].
Institutional systemic factors influencing nurses’ adherence to and compliance with patient-safety principles are as follows: the organizational patient-safety climate [ 21 ], workload, time pressure, encouragement by leaders and colleagues [ 22 , 23 , 24 ], level of ward performance [ 25 ], provision of education for the improvement of knowledge and skills [ 11 , 18 ], institutional procedures or protocols, and also communication between healthcare staff and patients [ 11 ]. In addition, personal motivation, resistance to change, feelings of autonomy, attitude toward innovation, and empowerment are personal factors that impact on the nurses’ adherence to patient-safety principles [ 26 ].
A theoretical framework for analysing risk and safety in healthcare practice has been devised by Vincent et al. (1998) [ 27 ] based on the Reason’s model of organizational accidents [ 28 ]. It combines ‘person-centred’ approaches, where the focus is on individual responsibility for the preservation of patients’ safety and prevention of their harm, and the ‘system-centred’ approach, which considers organizational factors as precursors for endangering patient safety [ 29 ]. According to this theoretical framework, initiatives aimed at the improvement of patient safety require systematic assessments and integrative interventions to target different elements in the hierarchy of the healthcare system, including patient, healthcare provider, task, work environment, and organization and management. This framework, and similar models for risk and safety management, can help with the analysis of patient harm, to identify probable pitfalls, as well as explore how to prevent future similar incidents [ 30 ].
Adherence to the principles of patient safety and the prevention and reduction of practice errors have been facilitated by technological solutions in recent years [ 31 , 32 ]; however, suboptimal quality and safety of care remain evident, indicating the need for improved understandings of the various factors and conditions that increase adherence in daily nursing practice [ 33 ]. Consequently, this review aimed to retrieve, explore, and synthesise factors evident in the international literature that influenced nurses’ adherence to patient-safety principles. Vincent’s framework was used for the classification of findings, in order to systematically present the findings and inform clinical practice.
2. Materials and Methods
2.1. design.
A systematic review was conducted. It is an explicit and clear method of data collection, systematic description, and synthesis of findings, to reach the study goal [ 34 , 35 , 36 ]. The review findings are presented narratively since heterogeneities in the methods, objectives, and results of studies that met the inclusion criteria did not lend themselves to meta-analysis. The Preferred Reporting Items Systematic Reviews and Meta-analysis (PRISMA) Statement (2009) was applied to inform this systematic review [ 36 ].
2.2. Search Methods
Search keywords were determined after team discussions, performing a pilot search in general and specialized databases, and consultation with a librarian. Key search terms relating to adherence to patient-safety principles by nurses were used to conduct a Boolean search. For operationalising the study concept, the definition of adherence as a behaviour carried out actively by people according to orders or advice was used [ 37 ]. The word adherence is used interchangeably with, and sometimes at the same time as, the word compliance, since both can indicate the outcome of care interactions between the healthcare provider and the caregiver [ 38 , 39 , 40 , 41 , 42 ]. However, adherence indicates responsibility and empowerment on the healthcare professional’s part to actively perform the expected behaviour compared to compliance that shows responsibility on the patient’s part to follow up the therapeutic regimen [ 43 , 44 ].
The search was limited to the time period of January 2010 to August 2019, in English scientific journals available through the following online databases: PubMed (including Medline), CINAHL, Scopus, Web of Science, PsycINFO, ProQuest, and EBSCO. In addition, the authors performed searches in Nordic and Finnish databases to improve the search coverage. To find relevant studies for inclusion in the data analysis and synthesis, inclusion criteria for selection were articles with a focus on adherence to patient-safety principles in clinical nursing interventions published in online peer-reviewed scientific journals. Articles on patients and other healthcare providers, or on non-clinical initiatives, or that had no exact relevance to adherence to patient-safety principles were excluded.
2.3. Search Outcome and Data Extraction
The authors (M.V., S.T., J.K., and F.V.M.) independently performed each step of the systematic review, holding frequent online discussions and making collective agreements on how to proceed through the review steps. Gray literature, such as unpublished dissertations and policy documents and cross-referencing from bibliographies, were assessed, to improve the search coverage. Guidance and support with the search process were obtained from the librarian, when needed. All authors independently screened the titles, abstracts, and full texts of the studies retrieved during the search process. In the cases where disagreements about the inclusion of selected studies occurred, discussions were held until a consensus was reached.
A data extraction table was used to collect data on the characteristics of studies. The table included the lead author’s name, publication year, country, design, sample size and setting, and information relating to adherence to patient-safety principles. Prior to the full data extraction, this table was pilot-tested with a few selected studies, to ensure that data relevant to the review aim and analysis would be appropriately gathered.
2.4. Quality Appraisal
The selected articles were appraised based on the appropriateness of the research structure using the evaluation tools provided by the Enhancing the QUAlity and Transparency of health Research (EQUATOR) website [ 45 ] and criteria outlined by Hawker et al. (2002) [ 46 ], addressing the study aim, research structure, theoretical/conceptual research framework, conclusion, and references. The appraisal tool appropriate to cross-sectional, observational and cohort studies such as the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) was used to evaluate the suitability of selected studies for inclusion in the final data synthesis and analysis. The researchers believed that the quality appraisal items for determining the inclusion of a study in the final dataset did not align to a scoring system; therefore, they used a yes/no system to answer the appraisal-tool items during the quality appraisal and held frequent discussions on the importance and quality of each article before making the final decision on the selection of studies for data analysis and synthesis.
2.5. Data Abstraction and Synthesis
The Vincent’s framework for analysing risk and safety in clinical practice [ 27 , 47 ] was used to organize and connect the review findings to the wider theoretical perspective of patient safety. This framework was developed based on the Reason’s organisational accident model [ 28 ]. Accordingly, issues in patient safety originate in various systemic features at different categories of patient, healthcare provider, task, work environment, and organisation and management [ 27 , 47 ]. The use of this framework helped with the description and categorisation of data retrieved and accommodated heterogeneities in the studies retrieved, with respect to method, samples, settings, and findings, facilitating the integrative presentation of the review findings. The authors (M.V., S.T., P.A.L., J.K., and F.V.M.) reviewed the included studies, to allocate the studies’ findings to each category, and used frequent discussions to reach a consensus.
3.1. Search Results and Study Selections
The thorough literature search using the key terms led to the retrieval of 10,855 articles. After deleting irrelevant and duplicate titles, 382 entered the abstract-reading phase. Each abstract was assessed by using the inclusion criteria, resulting in 84 possibly relevant articles. The full texts were obtained from Finnish and Norwegian libraries and were carefully read to select only those articles that had a precise focus on adherence to patient-safety principles during clinical nursing interventions by nurses. This resulted in the final six articles chosen for data analysis. Excluded studies were on adherence by other healthcare providers, rather than nurses, or had no exact relevance to patient-safety principles. The methodological quality of the selected articles was assessed during the full-text appraisal, and no article was excluded. In general, they had acceptable qualities with respect to study research structure, theoretical and conceptual research frameworks, and relevant findings to the review aim. Grey literature and the manual search in the reference lists of the selected studies led to no more articles being discovered for inclusion. Appendix A presents the search results, giving the number of articles located in each database. The Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) flowchart is shown in Figure 1 .
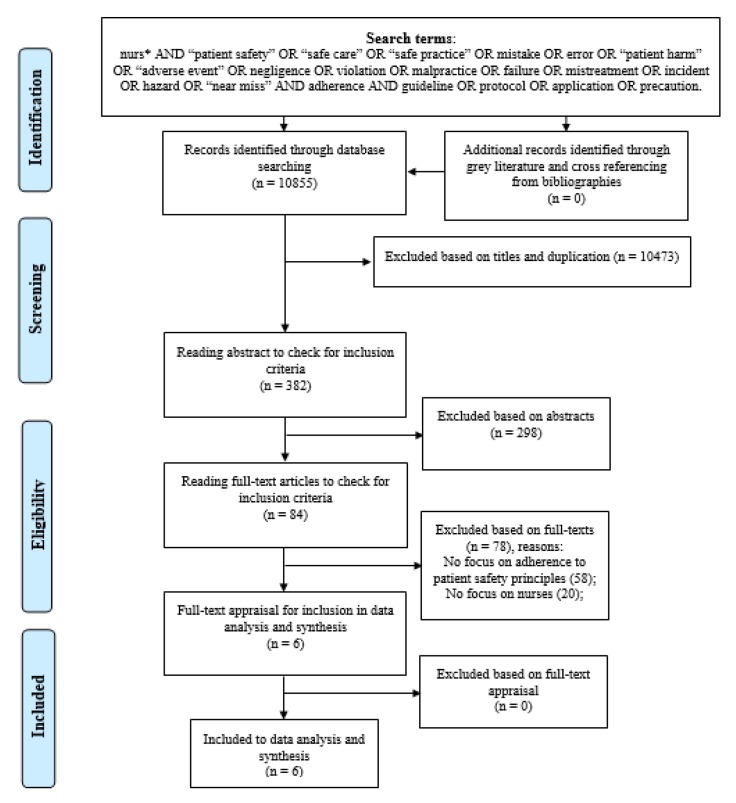
The study flow diagram according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA).
3.2. General Characteristics of the Selected Studies
The general characteristics of the selected studies ( n = 6) are presented in Table 1 . The studies were published from 2014 to 2019 and were conducted in Australia [ 48 ], Finland [ 49 ], Norway [ 50 ], South Korea [ 51 ], Sweden [ 52 ], and the UK [ 53 ].
Characteristics of selected studies for data analysis and synthesis.
PICU: paediatric intensive care unit; NICU: neonatal intensive care unit; ICU: intensive care unit.
Three studies used a survey design [ 50 , 51 , 52 ]; one study used an observational method [ 53 ]; one applied an observational intervention design [ 49 ]; and another one was a three-stage pre-post time-series study [ 48 ]. Except for one study [ 49 ] that was published in the Finnish language, all other articles were written in English.
Diverse foci were evident in the studies: adherence to patient-safety principles on the management of peripheral venous catheters [ 52 ], surgical hand rubbing instructions [ 49 ], double-checking policies of medicines’ preparation and administration [ 53 ], handover from the intensive care unit (ICU) to the cardiac ward [ 48 ], cardiac monitoring and surveillance standards [ 50 ], and care-associated infection precautions [ 51 ].
3.3. Findings of Studies with Connection to the Vincent’s Framework
The findings were classified based on the theoretical framework for analysing risk and safety in clinical practice developed by Vincent (1998, 2010) [ 27 , 47 ] and grouped by factors related to the patient, healthcare provider, task, work environment, and organisation and management. Variations in the findings within the selected studies related to the type of patient-safety principles or different clinical settings facilitated the description and synthesis of findings under the above-mentioned categories ( Figure 2 ).
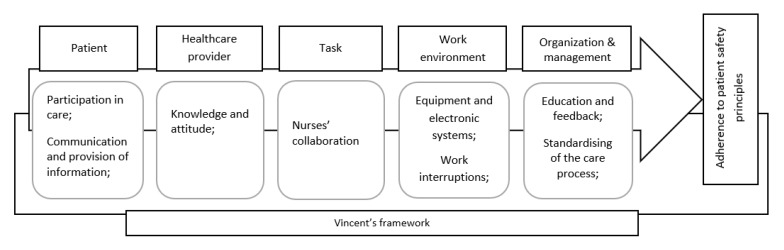
Schematic model of nurses’ adherence to patient-safety principles based on the Vincent’s framework.
3.3.1. Patient
This category was about the role of patients and how they could impact nurses’ adherence to patient-safety principles. For instance, errors made during medicines’ preparation and administration, and a deviation from medication safety principles by nurses were reported. The deviation with a high possibility of endangering patient safety happened where the parents of patients or their companions were left unobserved and unsupervised by nurses to administer medicines to patients. Unobserved or unsupervised administration contravenes the medicines management principle, which requires a nurse’s direct supervision; a crucial consideration for the prevention of abuse and patient avoidance of taking medicines as prescribed [ 53 ]. Moreover, in spite of the emphasis on patient participation in patient-safety activities, nursing handovers were delivered mainly outside the patient’s room [ 48 ], or no information was provided to patients regarding the purpose and process of cardiac monitoring [ 50 ]. These deviations could hinder patients’ active involvement in their own safe care. Additionally, the only communication line between patients and nurses was the call bell, and nurses rarely questioned patients about their pain or comfort. These identified issues represent missed opportunities for the nurses’ continuous observation role for early detection and prevention of harm during handovers from the ICU to the cardiac ward [ 48 ].
3.3.2. Healthcare Provider
This category described how nurses’ knowledge and attitudes were associated with their adherence to patient-safety principles. Variations in nurses’ adherence to patient-safety principles could be attributed to their varied levels of knowledge and attitudes. Examples included nurses’ incomplete adherence to infection-control principles, which encompassed the daily inspection of peripheral venous catheter sites, surgical hand rubbing, disinfection of hands, and the use of disposable gloves and aprons when exposed to patient excretions [ 49 , 51 , 52 ]. Other examples were related to the principles of medicines’ management: inappropriate speed of intravenous bolus, incorrect medicines’ preparation, administration at incorrect times, problematic labelling of flush syringes and administration of intravenous antibiotics without flushing, not receiving the medicines’ complete dose by patients, and incorrect mixing of medicines with diluent [ 53 ]. Lack of sufficient knowledge and skills regarding cardiac monitoring and surveillance standards were also evident, with incorrect placement of cardiac electrodes and/or skin preparation before the procedure leading to inconsistent monitoring, which could endanger patient safety [ 50 ]. Interestingly, being a newly graduated nurse with less time having passed since obtaining the nursing certificate was associated with better adherence to the peripheral venous catheter-care principles, possibly due to having more informatics skills and updated knowledge of nursing care and following up of rules set by senior nurses [ 52 ]. Additionally, negative attitudes and perceptions toward the significance of care standards, individual aesthetic manicure preferences, and the presence of eczema and skin wounds hindered adherence to the surgical hand rubbing protocol, thus having negative implications for patient safety [ 49 ].
3.3.3. Task
In this category, the association between the identity and type of nursing task and adherence to patient-safety principles by nurses was considered. The lowest adherence rates were evident in ‘independent’ medicine management tasks such as dose calculation, rate of administering intravenous bolus drugs, and labelling of flush syringes. On the other hand, a higher rate of adherence was reported for ‘cooperative’ tasks with higher levels of complexity, such as the double-checking of drugs for the actual administration of medicine to the patient [ 53 ]. Similarly, a higher number of nurses working and collaborating together in the ward was associated with a higher rate of adherence to infection-control precautions, including putting sharp articles into appropriate boxes, covering both the mouth and nose, and disinfection of hands after glove removal [ 51 ].
3.3.4. Work Environment
The effect of equipment and the workplace condition on adherence to patient-safety principles was reported in this category. The availability of equipment and electronic resources and digitalization increased the likelihood of adherence to patient safety principles related to medicine management [ 53 ], peripheral venous catheter care [ 52 ], and cardiac monitoring and surveillance [ 50 ]. Accordingly, a telemetry cover on cardiac telemetry and monitoring units helped with the prevention of nosocomial infection by preventing contamination of shared equipment [ 50 ]. Electronic resources and digitalization helped with reminding the daily inspection and information-sharing between nurses regarding peripheral venous catheter insertion sites [ 52 ]. The existence of an environmental space for preparation of medicines without interruptions helped nurses adhere more closely to double-checking instructions of preparation and administration on weekends, as compared with weekdays [ 53 ].
3.3.5. Organisation and Management
This category focused on collaboration between nurses and the leadership role in motivating nurses’ adherence to patient-safety principles. As an example, adherence to the surgical hand rubbing principles, including properly drying hands after alcohol hand rubbing and washing with water and soap, and alcohol hand rubbing up to elbows, was improved after the provision of feedback by nurse leaders [ 49 ]. Regular practical feedback processes, interaction opportunities and observation of peers and senior colleagues, and leadership motivated nurses’ adherence to daily inspection of the peripheral venous catheter site and the use of disposable gloves when handling peripheral venous catheters insertion sites [ 52 ]. Adherence to patient-safety principles by cardiac nurses was improved through feedback provision and informing nurses in the ICU of the type of nursing interventions conducted in cases of serious dysrhythmias and their outcomes [ 50 ].
The provision of a standard process for handover, such as the introduction of a validated handover tool, improved nurses’ readiness to receive patients from the ICU. It informed the preparation of the required equipment for care, enabled performance of handovers at the patient bedside, and involved patients in their care, while also assisting with attending patients’ needs, checking patients’ identity, and collecting data of their medical history and allergies. Further, the standardising of the handover process helped with the continuity of care plan by formalising discussions between nurses and assisting with removal of any ambiguities, so increasing awareness of risks to patient safety [ 48 ]. The higher adherence rate to standard precautions for infection control were found when there was a higher nurse-to-patient ratio indicating the association between workload and patient-safety management [ 51 ]. Similarly, the development of a local practice standard for cardiac monitoring and surveillance, as well as for assessing the eligibility of patients for admission to critical and non-critical telemetry sections, would improve adherence to patient-safety principles for the cardiac patient [ 50 ].
4. Discussion
This systematic review integrated current international knowledge through the categorization of factors affecting adherence to patient-safety principles by nurses to the elements of the Vincent’s framework (1998 and 2010) for analysing risk and safety in clinical practice [ 27 , 47 ].
In this review, leaving patients’ companions unsupervised during medicines’ administration, performing handovers outside patients’ rooms, and lack of the provision of information and appropriate communication with patients hindered patient participation in their understandings of their own care. Lack of engagement of patients in safe-care initiatives contravenes nurses’ adherence to patient-safety principles. Benefiting from patients’ participation requires understanding of how to improve the patient’s willingness to act as an active member of the healthcare team, development of practical guidelines for such an engagement with the consideration of patients and their relatives’ knowledge and skills of the care process, as well as definition of the role and provision of supervision and guidance by nurses. The assigned participation task should be communicated appropriately to the patient, have congruity with patients’ knowledge of nursing routines and their own implementation capacity, as well as be incorporated into routine care with the consideration of infrastructures and healthcare missions [ 14 , 54 , 55 ]. It has been suggested that planning and performing nursing care at the patient’s bedside can improve patient participation, reduce work interruptions [ 56 ], and consequently improve nurses’ adherence to safe care guidelines [ 11 ].
The findings of this review highlighted that nurses’ knowledge, perceptions, and attitudes influenced their adherence to patient-safety principles. Nurses have multiple roles and central responsibility to keep patients safe in the complex healthcare environment [ 57 , 58 ]. The effect of personal and professional values and attitudes on the consistency of adherence to patient safety by nurses has been shown to be more important than the effect of their workloads [ 22 ]. It is believed that individual factors such as nurses’ attitudes, perceptions, knowledge, and information seeking can facilitate or hinder the use of clinical practice guidelines by nurses and consequently endanger patient safety [ 11 , 26 ] through inconsistent adherence to patient-safety principles [ 59 ].
It was evident that collaborative tasks fostered nurses’ adherence to patient-safety principles. Improving nurses’ knowledge of tasks improves nurses’ adherence [ 60 ]. Moreover, the coordinated management approach and collaboration with team members enhance the effectiveness of patient-safety interventions due to the creation of a shared understanding of changes that should be made by all healthcare staff to improve the quality of care [ 61 , 62 ].
With regard to the work environment, the findings of this review highlighted how equipment and electronic systems could assist with sharing information between healthcare providers and enhance adherence to patient-safety principles. One part of the healthcare system’s commitment to patient safety is the preparation of appropriate work equipment [ 63 , 64 ]. Technology can support data security and facilitate nursing care through the provision of real-time and ubiquitous documentation, which is needed for professional interactions and collaboration [ 65 ]. Digital systems can reduce the time needed to perform nursing care and limit errors in drug administration, as well as improve nurses’ and patients’ satisfaction with care [ 66 , 67 ].
An appropriate work environment was characterised as one where nurses were less interrupted, and lower workloads improved adherence to patient-safety principles. An appropriate work environment is associated with better patient safety and less burnout. Workload and burnout act as negative mediators of safe care [ 68 , 69 ]. A work environment characterised by a heavy workload and mental pressure [ 23 , 24 , 70 ] and frequent disruptions [ 71 ] has been implicated in reducing nurses’ adherence to safety-related principles. There is an association between patient safety and the nurses’ work environment [ 39 , 72 , 73 ] and implementation of patient-safety principles to prevent errors and adverse events [ 26 , 74 ].
The findings of this review emphasized the role of regular education and provision of feedback to nurses. Taking responsibility for actions and behaviours through education and feedback is a crucial aspect of professional practice [ 75 ]. The empowerment of nurses to intervene based on care standards is an expectation of healthcare leaders which can be achieved through the development of the culture of patient safety [ 33 , 76 , 77 , 78 ], the implementation of educational programs, and timely feedback and reminders [ 79 , 80 , 81 ]. Further, the use of standard processes, supported by validated tools, guided nurses and facilitated their adherence to patient-safety principles. Usability, format, easy access of the contents of guidelines, and consideration of time, staffing, chain of communication, accuracy of practice, supplies of equipment, and logistics are the main advantages of guidelines that facilitate the implementation of safe care [ 26 , 82 ].
Limitations and Suggestions for Future Studies
In spite of the emphasis on adherence to patient-safety principles and patient-care outcomes, this study has directly focused on nurses’ adherence to patient-safety principles, which can impact our understandings of the variation of factors influencing this important concept. However, the wide nature of the search in the electronic databases and in various languages convinced the researchers that the study topic has been addressed appropriately and an answer based on the current knowledge can be provided. However, the limited number of studies that met the inclusion criteria for this review hinders the full exploration of the relationship between individual and systemic factors that impact on nurses’ adherence to patient-safety principles in inpatient and outpatient settings.
5. Conclusions
This review has shown that adherence to patient-safety principles was affected by numerous intersecting and complex factors. Variations in the studies’ aims, methods, and results hinder the formation of a determinant conclusion on how adherence to patient-safety principles can be improved. However, based on the review results, general indications are that improvement of nurses’ knowledge about patient safety, collaboration in performing tasks, reduction of workloads, provision of appropriate equipment and electronic systems for communication and sharing information, regular feedback in the workplace, and standardization of the care processes can help with enhancing nurses’ adherence to patient-safety principles. Future qualitative and quantitative studies are needed to better understand how to promote and mitigate adherence to safe-care principles by clinical nurses.
Acknowledgments
Nord University, Bodø, Norway has supported the publication of this manuscript through coverage of publication charges.
Search strategy and results based on each database.
Author Contributions
The authors contributed to the design and implementation of the research, to the analysis of the results and to the writing of the manuscript as follows; M.V., S.T., J.K., F.V.-M.: Conceptualization, Data curation, Formal analysis, Investigation, Methodology, Project administration, Resources, Software; M.V., S.T., J.K., F.V.-M., P.A.L.: Writing—original draft, Writing—review and editing. All authors have read and agreed to the published version of the manuscript.
This research received no external funding.
Conflicts of Interest
The authors have no conflicts of interest to declare.
- 1. World Heath Organization (WHO) Patient Safety. [(accessed on 24 December 2019)];2019 Available online: https://www.who.int/patientsafety/en/
- 2. Harvard Global Health Institute Patient Safety: A Major Public Health Challenge. [(accessed on 8 March 2020)]; Available online: https://globalhealth.harvard.edu/qualitypowerpoint .
- 3. Adler L., Yi D., Li M., McBroom B., Hauck L., Sammer C., Jones C., Shaw T., Classen D. Impact of Inpatient Harms on Hospital Finances and Patient Clinical Outcomes. J. Patient Saf. 2018;14:67–73. doi: 10.1097/PTS.0000000000000171. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 4. Slawomirski L., Auraaen A., Klazinga N.S. The Economics of Patient Safety. [(accessed on 19 March 2020)]; Available online: https://www.oecd-ilibrary.org/social-issues-migration-health/the-economics-of-patient-safety_5a9858cd-en .
- 5. Rodziewicz T.L., Hipskind J.E. StatPearls. StatPearls Publishing; Treasure Island, FL, USA: 2020. Medical Error Prevention. [ Google Scholar ]
- 6. Emanuel L., Berwick D., Conway J., Combes J., Hatlie M., Leape L., Reason P., Schyve P., Vincent C., Walton M. Advances in Patient Safety: New Directions and Alternative Approaches. Agency for Healthcare Research and Quality; Rockville, MD, USA: 2008. What Exactly is Patient Safety. [ PubMed ] [ Google Scholar ]
- 7. Sibal A., Uberoi R.S., Malani A. An approach to improve patient safety and quality beyond accreditation. World Hosp. Health Serv. 2016;52:10–12. [ PubMed ] [ Google Scholar ]
- 8. Mitchell P. Patient Safety and Quality: An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality; Rockville, MD, USA: 2008. Defining Patient Safety and Quality Care. [ PubMed ] [ Google Scholar ]
- 9. Kanerva A., Kivinen T., Lammintakanen J. Collaborating with nurse leaders to develop patient safety practices. Leadersh Health Serv. 2017;30:249–262. doi: 10.1108/LHS-05-2016-0022. [ DOI ] [ PubMed ] [ Google Scholar ]
- 10. Dixon-Woods M. Why is Patient Safety so Hard? A Selective Review of Ethnographic Studies. J. Health Serv. Res. Policy. 2010;15:11–16. doi: 10.1258/jhsrp.2009.009041. [ DOI ] [ PubMed ] [ Google Scholar ]
- 11. Lin F., Gillespie B.M., Chaboyer W., Li Y., Whitelock K., Morley N., Morrissey S., O’Callaghan F., Marshall A.P. Preventing surgical site infections: Facilitators and barriers to nurses’ adherence to clinical practice guidelines—A qualitative study. J. Clin. Nurs. 2019;28:1643–1652. doi: 10.1111/jocn.14766. [ DOI ] [ PubMed ] [ Google Scholar ]
- 12. Sermeus W. Understanding the role of nurses in patient safety: From evidence to policy with RN4CAST. BMC Nurs. 2016;15:1 [ Google Scholar ]
- 13. Henneman E.A. Recognizing the Ordinary as Extraordinary: Insight into the “Way We Work” to Improve Patient Safety Outcomes. Am. J. Crit. Care. 2017;26:272–277. doi: 10.4037/ajcc2017812. [ DOI ] [ PubMed ] [ Google Scholar ]
- 14. Vaismoradi M., Jordan S., Kangasniemi M. Patient participation in patient safety and nursing input—a systematic review. J. Clin. Nurs. 2015;24:627–639. doi: 10.1111/jocn.12664. [ DOI ] [ PubMed ] [ Google Scholar ]
- 15. International Council of Nurses (ICN) Patient Safety-ICN Position. [(accessed on 24 December 2019)];2019 Available online: https://www.icn.ch/sites/default/files/inline-files/D05_Patient_Safety_0.pdf .
- 16. Rashvand F., Ebadi A., Vaismoradi M., Salsali M., Yekaninejad M.S., Griffiths P., Sieloff C. The assessment of safe nursing care: Development and psychometric evaluation. J. Nurs. Manag. 2017;25:22–36. doi: 10.1111/jonm.12424. [ DOI ] [ PubMed ] [ Google Scholar ]
- 17. Vaismoradi M., Salsali M., Turunen H., Bondas T. A qualitative study on Iranian nurses’ experiences and perspectives on how to provide safe care in clinical practice. J. Res. Nurs. 2013;18:351–365. doi: 10.1177/1744987112451578. [ DOI ] [ Google Scholar ]
- 18. Efstathiou G., Papastavrou E., Raftopoulos V., Merkouris A. Factors influencing nurses’ compliance with Standard Precautions in order to avoid occupational exposure to microorganisms: A focus group study. BMC Nurs. 2011;10:1. doi: 10.1186/1472-6955-10-1. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 19. Haynes R.B., Sackett D.L., Taylor D.W. Compliance in Health Care. John Hopkins University Press; Baltimore, MD, USA: 1979. [ Google Scholar ]
- 20. Playle J.F., Keeley P. Non-compliance and professional power. J. Adv. Nurs. 1998;27:304–311. doi: 10.1046/j.1365-2648.1998.00530.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 21. Hessels A.J., Larson E.L. Relationship between patient safety climate and standard precaution adherence: A systematic review of the literature. J. Hosp. Infect. 2016;92:349–362. doi: 10.1016/j.jhin.2015.08.023. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 22. Jam R., Mesquida J., Hernández Ó., Sandalinas I., Turégano C., Carrillo E., Pedragosa R., Valls J., Parera A., Ateca B., et al. Nursing workload and compliance with non-pharmacological measures to prevent ventilator-associated pneumonia: A multicentre study. Nurs. Crit. Care. 2018;23:291–298. doi: 10.1111/nicc.12380. [ DOI ] [ PubMed ] [ Google Scholar ]
- 23. Jimmieson N.L., Tucker M.K., White K.M., Liao J., Campbell M., Brain D., Page K., Barnett A.G., Graves N. The role of time pressure and different psychological safety climate referents in the prediction of nurses’ hand hygiene compliance. Saf. Sci. 2016;82:29–43. doi: 10.1016/j.ssci.2015.08.015. [ DOI ] [ Google Scholar ]
- 24. Zhang S., Kong X., Lamb K.V., Wu Y. High nursing workload is a main associated factor of poor hand hygiene adherence in Beijing, China: An observational study. Int. J. Nurs. Pract. 2019;25:e12720. doi: 10.1111/ijn.12720. [ DOI ] [ PubMed ] [ Google Scholar ]
- 25. Schutijser B., Klopotowska J.E., Jongerden I., Spreeuwenberg P., Wagner C., de Bruijne M. Nurse compliance with a protocol for safe injectable medication administration: Comparison of two multicentre observational studies. BMJ Open. 2018;8:e019648. doi: 10.1136/bmjopen-2017-019648. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 26. Jun J., Kovner C.T., Stimpfel A.W. Barriers and facilitators of nurses’ use of clinical practice guidelines: An integrative review. Int. J. Nurs. Stud. 2016;60:54–68. doi: 10.1016/j.ijnurstu.2016.03.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 27. Vincent C., Taylor-Adams S., Stanhope N. Framework for analysing risk and safety in clinical medicine. BMJ. 1998;316:1154–1157. doi: 10.1136/bmj.316.7138.1154. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 28. Reason J. Human error: Models and management. BMJ. 2000;320:768–770. doi: 10.1136/bmj.320.7237.768. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 29. van Beuzekom M., Boer F., Akerboom S., Hudson P. Patient safety: Latent risk factors. BJA Br. J. Anaesth. 2010;105:52–59. doi: 10.1093/bja/aeq135. [ DOI ] [ PubMed ] [ Google Scholar ]
- 30. Vincent C., Burnett S., Carthey J. Safety measurement and monitoring in healthcare: A framework to guide clinical teams and healthcare organisations in maintaining safety. BMJ Qual. Saf. 2014;23:670–677. doi: 10.1136/bmjqs-2013-002757. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 31. Kutney-Lee A., Kelly D. The effect of hospital electronic health record adoption on nurse-assessed quality of care and patient safety. J. Nurs. Adm. 2011;41:466–472. doi: 10.1097/NNA.0b013e3182346e4b. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 32. Strudwick G., Reisdorfer E., Warnock C., Kalia K., Sulkers H., Clark C., Booth R. Factors Associated With Barcode Medication Administration Technology That Contribute to Patient Safety: An Integrative Review. J. Nurs. Care Qual. 2018;33:79–85. doi: 10.1097/NCQ.0000000000000270. [ DOI ] [ PubMed ] [ Google Scholar ]
- 33. Hessels A.J., Wurmser T. Relationship among safety culture, nursing care, and Standard Precautions adherence. Am. J. Infect. Control. 2019 doi: 10.1016/j.ajic.2019.11.008. [ DOI ] [ PubMed ] [ Google Scholar ]
- 34. Evans D. Systematic reviews of nursing research. Intensive Crit. Care Nurs. 2001;17:51–57. doi: 10.1054/iccn.2000.1550. [ DOI ] [ PubMed ] [ Google Scholar ]
- 35. Higgins J.P.T., Green S.E. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1 [updated March 2011] [(accessed on 19 March 2020)];2011 Available online: http://handbook-5-1.cochrane.org/
- 36. Liberati A., Altman D.G., Tetzlaff J., Mulrow C., Gøtzsche P.C., Ioannidis J.P.A., Clarke M., Devereaux P.J., Kleijnen J., Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ. 2009;339:b2700. doi: 10.1136/bmj.b2700. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 37. Gardner C.L. Adherence: A concept analysis. Int. J. Nurs. Knowl. 2015;26:96–101. doi: 10.1111/2047-3095.12046. [ DOI ] [ PubMed ] [ Google Scholar ]
- 38. Brown M.T., Bussell J., Dutta S., Davis K., Strong S., Mathew S. Medication Adherence: Truth and Consequences. Am. J. Med. Sci. 2016;351:387–399. doi: 10.1016/j.amjms.2016.01.010. [ DOI ] [ PubMed ] [ Google Scholar ]
- 39. Kim J.M., Suarez-Cuervo C., Berger Z., Lee J., Gayleard J., Rosenberg C., Nagy N., Weeks K., Dy S. Evaluation of Patient and Family Engagement Strategies to Improve Medication Safety. Patient. 2018;11:193–206. doi: 10.1007/s40271-017-0270-8. [ DOI ] [ PubMed ] [ Google Scholar ]
- 40. Lam W.Y., Fresco P. Medication Adherence Measures: An Overview. Biomed. Res. Int. 2015;2015:217047. doi: 10.1155/2015/217047. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 41. Roter D.L., Wolff J., Wu A., Hannawa A.F. Patient and family empowerment as agents of ambulatory care safety and quality. BMJ Qual. Saf. 2017;26:508–512. doi: 10.1136/bmjqs-2016-005489. [ DOI ] [ PubMed ] [ Google Scholar ]
- 42. Sharma A.E., Rivadeneira N.A., Barr-Walker J., Stern R.J., Johnson A.K., Sarkar U. Patient Engagement in Health Care Safety: An Overview Of Mixed-Quality Evidence. Health Aff. 2018;37:1813–1820. doi: 10.1377/hlthaff.2018.0716. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 43. Bissonnette J.M. Adherence: A concept analysis. J. Adv. Nurs. 2008;63:634–643. doi: 10.1111/j.1365-2648.2008.04745.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 44. Kyngäs H., Duffy M.E., Kroll T. Conceptual analysis of compliance. J. Clin. Nurs. 2000;9:5–12. doi: 10.1046/j.1365-2702.2000.00309.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 45. EQUATOR Network Enhancing the QUAlity and Transparency of health Research. [(accessed on 4 November 2019)];2019 Available online: http://www.equator-network.org/
- 46. Hawker S., Payne S., Kerr C., Hardey M., Powell J. Appraising the evidence: Reviewing disparate data systematically. Qual. Health Res. 2002;12:1284–1299. doi: 10.1177/1049732302238251. [ DOI ] [ PubMed ] [ Google Scholar ]
- 47. Vincent C. Patient Safety. 2nd ed. Wiley-Blackwell; Oxford, UK: 2010. [ Google Scholar ]
- 48. Graan S.M., Botti M., Wood B., Redley B. Nursing handover from ICU to cardiac ward: Standardised tools to reduce safety risks. Aust. Crit. Care. 2016;29:165–171. doi: 10.1016/j.aucc.2015.09.002. [ DOI ] [ PubMed ] [ Google Scholar ]
- 49. Rintala E., Laurikainen E., Kaarto A.-M., Routamaa M. Adherence to surgical hand rubbing directives in a hospital district of Southwest Finland. Suomen Lääkärilehti. 2014 doi: 10.3109/23744235.2015.1089591. [ DOI ] [ PubMed ] [ Google Scholar ]
- 50. Fålun N., Oterhals K., Pettersen T., Brørs G., Olsen S.S., Norekvål T.M., TELMON-NOR Investigators Cardiovascular nurses’ adherence to practice standards in in-hospital telemetry monitoring. Nurs. Crit. Care. 2020;25:37–44. doi: 10.1111/nicc.12425. [ DOI ] [ PubMed ] [ Google Scholar ]
- 51. Lim J.-H., Ahn J.-W., Son Y.-J. Association between Hospital Nurses’ Perception of Patient Safety Management and Standard Precaution Adherence: A Cross-Sectional Study. Int. J. Environ. Res. Public Health. 2019;16:4744. doi: 10.3390/ijerph16234744. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 52. Förberg U., Wallin L., Johansson E., Ygge B.-M., Backheden M., Ehrenberg A. Relationship between work context and adherence to a clinical practice guideline for peripheral venous catheters among registered nurses in pediatric care. Worldviews Evid. Based Nurs. 2014;11:227–239. doi: 10.1111/wvn.12046. [ DOI ] [ PubMed ] [ Google Scholar ]
- 53. Alsulami Z., Choonara I., Conroy S. Paediatric nurses’ adherence to the double-checking process during medication administration in a children’s hospital: An observational study. J. Adv. Nurs. 2014;70:1404–1413. doi: 10.1111/jan.12303. [ DOI ] [ PubMed ] [ Google Scholar ]
- 54. Ijkema R., Langelaan M., van de Steeg L., Wagner C. Do patient characteristics influence nursing adherence to a guideline for preventing delirium? J. Nurs. Scholarsh. 2014;46:147–156. doi: 10.1111/jnu.12067. [ DOI ] [ PubMed ] [ Google Scholar ]
- 55. Tobiano G., Bucknall T., Marshall A., Guinane J., Chaboyer W. Nurses’ views of patient participation in nursing care. J. Adv. Nurs. 2015;71:2741–2752. doi: 10.1111/jan.12740. [ DOI ] [ PubMed ] [ Google Scholar ]
- 56. Malfait S., Eeckloo K., Van Biesen W., Van Hecke A. The effectiveness of bedside handovers: A multilevel, longitudinal study of effects on nurses and patients. J. Adv. Nurs. 2019;75:1690–1701. doi: 10.1111/jan.13954. [ DOI ] [ PubMed ] [ Google Scholar ]
- 57. Cathro H. Navigating Through Chaos: Charge Nurses and Patient Safety. J. Nurs. Adm. 2016;46:208–214. doi: 10.1097/NNA.0000000000000326. [ DOI ] [ PubMed ] [ Google Scholar ]
- 58. Gaffney T.A., Hatcher B.J., Milligan R. Nurses’ role in medical error recovery: An integrative review. J. Clin. Nurs. 2016;25:906–917. doi: 10.1111/jocn.13126. [ DOI ] [ PubMed ] [ Google Scholar ]
- 59. Ribeiro L., Fernandes G.C., Souza E.G.d., Souto L.C., Santos A.S.P.D., Bastos R.R. Safe surgery checklist: Filling adherence, inconsistencies, and challenges. Rev. Col. Bras. Cir. 2019;46:e20192311. doi: 10.1590/0100-6991e-20192311. [ DOI ] [ PubMed ] [ Google Scholar ]
- 60. Simons P.A.M., Houben R., Benders J., Pijls-Johannesma M., Vandijck D., Marneffe W., Backes H., Groothuis S. Does compliance to patient safety tasks improve and sustain when radiotherapy treatment processes are standardized? Eur. J. Oncol. Nurs. 2014;18:459–465. doi: 10.1016/j.ejon.2014.05.003. [ DOI ] [ PubMed ] [ Google Scholar ]
- 61. Manser T. Teamwork and patient safety in dynamic domains of healthcare: A review of the literature. Acta Anaesthesiol. Scand. 2009;53:143–151. doi: 10.1111/j.1399-6576.2008.01717.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 62. O’Brien B., Graham M.M., Kelly S.M. Exploring nurses’ use of the WHO safety checklist in the perioperative setting. J. Nurs. Manag. 2017;25:468–476. doi: 10.1111/jonm.12428. [ DOI ] [ PubMed ] [ Google Scholar ]
- 63. Massey D., Chaboyer W., Anderson V. What factors influence ward nurses’ recognition of and response to patient deterioration? An integrative review of the literature. Nurs. Open. 2016;4:6–23. doi: 10.1002/nop2.53. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 64. Ross C., Rogers C., King C. Safety culture and an invisible nursing workload. Collegian. 2019;26:1–7. doi: 10.1016/j.colegn.2018.02.002. [ DOI ] [ Google Scholar ]
- 65. Tunlind A., Granström J., Engström Å. Nursing care in a high-technological environment: Experiences of critical care nurses. Intensive Crit. Care Nurs. 2015;31:116–123. doi: 10.1016/j.iccn.2014.07.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 66. Lee T.-Y., Sun G.-T., Kou L.-T., Yeh M.-L. The use of information technology to enhance patient safety and nursing efficiency. Technol. Health Care. 2017;25:917–928. doi: 10.3233/THC-170848. [ DOI ] [ PubMed ] [ Google Scholar ]
- 67. Pirinen H., Kauhanen L., Danielsson-Ojala R., Lilius J., Tuominen I., Díaz Rodríguez N., Salanterä S. Registered Nurses’ Experiences with the Medication Administration Process. Adv. Nurs. 2015:941589. doi: 10.1155/2015/941589. [ DOI ] [ Google Scholar ]
- 68. Liu X., Zheng J., Liu K., Baggs J.G., Liu J., Wu Y., You L. Hospital nursing organizational factors, nursing care left undone, and nurse burnout as predictors of patient safety: A structural equation modeling analysis. Int. J. Nurs. Stud. 2018;86:82–89. doi: 10.1016/j.ijnurstu.2018.05.005. [ DOI ] [ PubMed ] [ Google Scholar ]
- 69. Usher K., Woods C., Parmenter G., Hutchinson M., Mannix J., Power T., Chaboyer W., Latimer S., Mills J., Siegloff L., et al. Self-reported confidence in patient safety knowledge among Australian undergraduate nursing students: A multi-site cross-sectional survey study. Int. J. Nurs. Stud. 2017;71:89–96. doi: 10.1016/j.ijnurstu.2017.03.006. [ DOI ] [ PubMed ] [ Google Scholar ]
- 70. Hall L.H., Johnson J., Watt I., Tsipa A., O’Connor D.B. Healthcare Staff Wellbeing, Burnout, and Patient Safety: A Systematic Review. PLoS ONE. 2016;11:e0159015. doi: 10.1371/journal.pone.0159015. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 71. Schutijser B.C.F.M., Klopotowska J.E., Jongerden I.P., Spreeuwenberg P.M.M., De Bruijne M.C., Wagner C. Interruptions during intravenous medication administration: A multicentre observational study. J. Adv. Nurs. 2019;75:555–562. doi: 10.1111/jan.13880. [ DOI ] [ PubMed ] [ Google Scholar ]
- 72. Havaei F., MacPhee M., Lee S.E. The effect of violence prevention strategies on perceptions of workplace safety: A study of medical-surgical and mental health nurses. J. Adv. Nurs. 2019;75:1657–1666. doi: 10.1111/jan.13950. [ DOI ] [ PubMed ] [ Google Scholar ]
- 73. Manapragada A., Bruk-Lee V., Thompson A.H., Heron L.M. When safety climate is not enough: Examining the moderating effects of psychosocial hazards on nurse safety performance. J. Adv. Nurs. 2019;75:1207–1218. doi: 10.1111/jan.13911. [ DOI ] [ PubMed ] [ Google Scholar ]
- 74. Kim J., Bates D.W. Medication administration errors by nurses: Adherence to guidelines. J. Clin. Nurs. 2013;22:590–598. doi: 10.1111/j.1365-2702.2012.04344.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 75. Aveling E.-L., Parker M., Dixon-Woods M. What is the role of individual accountability in patient safety? A multi-site ethnographic study. Sociol. Health Illn. 2016;38:216–232. doi: 10.1111/1467-9566.12370. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 76. DiCuccio M.H. The Relationship Between Patient Safety Culture and Patient Outcomes: A Systematic Review. J. Patient Saf. 2015;11:135–142. doi: 10.1097/PTS.0000000000000058. [ DOI ] [ PubMed ] [ Google Scholar ]
- 77. Gurková E., Zeleníková R., Friganovic A., Uchmanowicz I., Jarošová D., Papastavrou E., Žiaková K. Hospital safety climate from nurses’ perspective in four European countries. Int. Nurs. Rev. 2019 doi: 10.1111/inr.12561. [ DOI ] [ PubMed ] [ Google Scholar ]
- 78. Hessels A.J., Genovese-Schek V., Agarwal M., Wurmser T., Larson E.L. Relationship between patient safety climate and adherence to standard precautions. Am. J. Infect. Control. 2016;44:1128–1132. doi: 10.1016/j.ajic.2016.03.060. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 79. Doronina O., Jones D., Martello M., Biron A., Lavoie-Tremblay M. A Systematic Review on the Effectiveness of Interventions to Improve Hand Hygiene Compliance of Nurses in the Hospital Setting. J. Nurs. Scholarsh. 2017;49:143–152. doi: 10.1111/jnu.12274. [ DOI ] [ PubMed ] [ Google Scholar ]
- 80. Martos-Cabrera M.B., Mota-Romero E., Martos-García R., Gómez-Urquiza J.L., Suleiman-Martos N., Albendín-García L., Cañadas-De la Fuente G.A. Hand Hygiene Teaching Strategies among Nursing Staff: A Systematic Review. Int. J. Environ. Res. Public Health. 2019;16:3039. doi: 10.3390/ijerph16173039. [ DOI ] [ PMC free article ] [ PubMed ] [ Google Scholar ]
- 81. Shimoni Z., Kama N., Mamet Y., Glick J., Dusseldorp N., Froom P. Empowering surgical nurses improves compliance rates for antibiotic prophylaxis after caesarean birth. J. Adv. Nurs. 2009;65:2345–2349. doi: 10.1111/j.1365-2648.2009.05096.x. [ DOI ] [ PubMed ] [ Google Scholar ]
- 82. Leotsakos A., Zheng H., Croteau R., Loeb J.M., Sherman H., Hoffman C., Morganstein L., O’Leary D., Bruneau C., Lee P., et al. Standardization in patient safety: The WHO High 5s project. Int. J. Qual. Health Care. 2014;26:109–116. doi: 10.1093/intqhc/mzu010. [ DOI ] [ PubMed ] [ Google Scholar ]
- View on publisher site
- PDF (1.0 MB)
- Collections
Similar articles
Cited by other articles, links to ncbi databases.
- Download .nbib .nbib
- Format: AMA APA MLA NLM
Add to Collections
Nurses' continuing professional development: A systematic literature review
Affiliations.
- 1 Clínica Universidad de Navarra, Avenida Pío XII, 31008, Pamplona, Navarra, Spain; IdiSNA, Navarra Institute for Health Research, Pamplona, Spain. Electronic address: [email protected].
- 2 IdiSNA, Navarra Institute for Health Research, Pamplona, Spain; University of Navarra, Faculty of Nursing, Calle Irunlarrea 1, 31008, Pamplona, Navarra, Spain. Electronic address: [email protected].
- 3 IdiSNA, Navarra Institute for Health Research, Pamplona, Spain; University of Navarra, Faculty of Nursing, Calle Irunlarrea 1, 31008, Pamplona, Navarra, Spain. Electronic address: [email protected].
- PMID: 33422973
- DOI: 10.1016/j.nepr.2020.102963
Nurses' continuing professional development (CPD) improves the quality of nursing care, patients' safety, nurses' satisfaction and healthcare costs. However, evidence has shown that nurses do not always participate in their CPD and that CPD does not always address nurses' real needs. To examine this issue, a systematic review of the literature on nurses' experiences regarding their CPD in the clinical context was carried out. The studies selected for this review (n = 9) were analyzed thematically, through which three themes were identified: The relevance of CPD to nurses; the intrinsic and extrinsic motivations of nurses to participate in CPD; and the specific needs of nurses to participate in CPD. The findings of this review highlight that nurses' experiences regarding their CPD is a key issue that has not been deeply studied. For nurses, their CPD continues throughout their professional career, and keeping their knowledge and skills up to date is important. The goals, motivations and needs that nurses may have to lead and participate in their CPD may vary according to their age and position. Organizations should consider nurses' specific professional situation as well as their actual needs to boost their CPD through different approaches and enhance nurses' retention at hospitals.
Keywords: Continuing professional development; Interpretive synthesis; Literature review; Nurse/nursing; Organizational support.
Copyright © 2020 Elsevier Ltd. All rights reserved.
Publication types
- Systematic Review
- Education, Nursing, Continuing*
- Motivation*
- Nursing Staff / education*
- Nursing Staff / psychology*
- Staff Development
- Systematic review
- Open access
- Published: 30 September 2024
Effects of implementation strategies on nursing practice and patient outcomes: a comprehensive systematic review and meta-analysis
- Guillaume Fontaine ORCID: orcid.org/0000-0002-7806-814X 1 , 2 , 3 , 4 ,
- Billy Vinette 5 , 6 ,
- Charlene Weight 1 ,
- Marc-André Maheu-Cadotte 5 ,
- Andréane Lavallée 7 ,
- Marie-France Deschênes 5 , 8 ,
- Alexandra Lapierre 9 ,
- Sonia A. Castiglione 1 , 10 ,
- Gabrielle Chicoine 6 , 11 ,
- Geneviève Rouleau 12 , 13 ,
- Nikolas Argiropoulos 3 ,
- Kristin Konnyu 14 ,
- Meagan Mooney 1 ,
- Christine E. Cassidy 15 , 16 ,
- Tanya Mailhot 5 , 17 ,
- Patrick Lavoie 5 , 17 ,
- Catherine Pépin 18 ,
- Sylvie Cossette 5 , 17 ,
- Marie-Pierre Gagnon 9 , 19 ,
- Sonia Semenic 1 , 10 ,
- Nicola Straiton 20 &
- Sandy Middleton 20 , 21
Implementation Science volume 19 , Article number: 68 ( 2024 ) Cite this article
4089 Accesses
11 Altmetric
Metrics details
Implementation strategies targeting individual healthcare professionals and teams, such as audit and feedback, educational meetings, opinion leaders, and reminders, have demonstrated potential in promoting evidence-based nursing practice. This systematic review examined the effects of the 19 Cochrane Effective Practice and Organization Care (EPOC) healthcare professional-level implementation strategies on nursing practice and patient outcomes.
A systematic review was conducted following the Cochrane Handbook, with six databases searched up to February 2023 for randomized studies and non-randomized controlled studies evaluating the effects of EPOC implementation strategies on nursing practice. Study selection and data extraction were performed in Covidence. Random-effects meta-analyses were conducted in RevMan, while studies not eligible for meta-analysis were synthesized narratively based on the direction of effects. The quality of evidence was assessed using GRADE.
Out of 21,571 unique records, 204 studies (152 randomized, 52 controlled, non-randomized) enrolling 36,544 nurses and 340,320 patients were included. Common strategies (> 10% of studies) were educational meetings, educational materials, guidelines, reminders, audit and feedback, tailored interventions, educational outreach, and opinion leaders. Implementation strategies as a whole improved clinical practice outcomes compared to no active intervention, despite high heterogeneity. Group and individual education, patient-mediated interventions, reminders, tailored interventions and opinion leaders had statistically significant effects on clinical practice outcomes. Individual education improved nurses’ attitude, knowledge, perceived control, and skills, while group education also influenced perceived social norms. Although meta-analyses indicate a small, non-statistically significant effect of multifaceted versus single strategies on clinical practice, the narrative synthesis of non-meta-analyzed studies shows favorable outcomes in all studies comparing multifaceted versus single strategies. Group and individual education, as well as tailored interventions, had statistically significant effects on patient outcomes.
Conclusions
Multiple types of implementation strategies may enhance evidence-based nursing practice, though effects vary due to strategy complexity, contextual factors, and variability in outcome measurement. Some evidence suggests that multifaceted strategies are more effective than single component strategies. Effects on patient outcomes are modest. Healthcare organizations and implementation practitioners may consider employing multifaceted, tailored strategies to address local barriers, expand the use of underutilized strategies, and assess the long-term impact of strategies on nursing practice and patient outcomes.
Trial registration
PROSPERO CRD42019130446.
Peer Review reports
Contributions to the literature
This is the first systematic review consolidating evidence on the effects of the 19 Cochrane Effective Practice and Organization of Care (EPOC) healthcare professional-level implementation strategies on nursing practice and patient outcomes.
It identifies effective strategies such as educational meetings and materials, opinion leaders, strategies tailored to context-specific barriers and facilitators, and reminders.
It illustrates the effects of strategies on determinants of nurses’ behaviors, including attitude, perceived behavioral control, and social norms.
It identifies the need for more high-quality studies evaluating underutilized strategies such as local consensus processes, patient-reported outcome measures, and continuous quality improvement, especially in low- and middle-income countries.
Nurses, comprising 59% of the global healthcare workforce, play a pivotal role in delivering both autonomous and collaborative care across the spectrum of healthcare services [ 1 , 2 ]. Their contributions are essential for achieving the United Nations’ 2030 Sustainable Development Goals (SDGs), particularly in ensuring healthy lives and promoting well-being for people of all ages [ 3 , 4 ]. Nurses are indispensable in providing comprehensive primary healthcare [ 5 ], ensuring quality care, and maintaining patient safety through clinical decision-making [ 6 ]. Given their central role in healthcare delivery, promoting the adoption of evidence-based practices among nurses is a global imperative to enhance patient outcomes and advance health equity [ 7 , 8 ]. The range of nursing practices is vast and can include administering medication, assessing illnesses, conducting tests and screenings, documenting care, practicing hand hygiene and other infection prevention measures, offering vaccinations, and providing counseling and advice on health behaviors [ 9 ].
The successful adoption and sustained use of evidence-based practices by nurses is influenced by a multitude of factors spanning individual, sociocultural, and environmental levels [ 9 , 10 , 11 , 12 , 13 ], as documented in implementation science determinant frameworks such as the Theoretical Domains Framework (TDF) [ 14 ]. These factors can either hinder or facilitate implementation and encompass challenges such as lack of knowledge, unfavorable social norms, workflow or process issues, ineffective teamwork or leadership, and inadequate institutional support [ 9 , 10 , 11 , 12 , 13 , 15 ]. Implementation science has generated a wealth of evidence on strategies that can overcome these multilevel barriers, fostering behavior change and promoting the adoption of best practices across various clinical contexts [ 16 , 17 , 18 ]. Implementation strategies—the specific methods/actions to promote the adoption of evidence-based practices—aim to produce change in nurses’ behaviors or the clinical environments in which they operate, or both [ 19 , 20 , 21 ].
Implementation strategy taxonomies have been developed to characterize intervention components aimed at promoting evidence uptake, including the Cochrane Effective Practice and Organisation of Care (EPOC) Taxonomy [ 22 ]. The EPOC Taxonomy includes 19 professional implementation strategies, targeting individual healthcare professionals and team behaviors, including audit and feedback, clinical practice guidelines, communities of practice, educational materials, local opinion leaders, printed educational materials, and reminders [ 22 ]. Multifaceted strategies, or implementation interventions, combine several of these strategies to address multiple barriers to implementation simultaneously [ 23 , 24 ]. Investigating the effectiveness of multifaceted versus single component strategies is crucial for identifying the most efficient methods to promote evidence-based practices, optimizing resource use, and enhancing patient outcomes [ 23 ].
Studies examining the effects of implementation strategies show small to moderate impacts on changing health professionals’ behaviors, with few providing evidence of a significant change in patient outcomes [ 25 ]. Systematic reviews have investigated the effects of audit and feedback [ 17 ], local opinion leaders [ 26 ], printed educational materials [ 27 ], strategies leveraging information and communication technologies [ 28 , 29 , 30 , 31 , 32 ], and reminders [ 33 ] on professional practice and patient outcomes. Specifically in nursing, two recent systematic reviews explored the effects of implementation strategies on the uptake of clinical practice guidelines by nurses and demonstrated positive effects on nursing practice and patient outcomes [ 34 , 35 ]. However, to our knowledge, no systematic review and meta-analysis has been conducted to consolidate evidence on the effects of the full range of EPOC healthcare professional-level implementation strategies on nurses’ practice and patient outcomes. Furthermore, no previous review has examined quantitatively the effects of implementation strategies on key determinants of nurses’ behaviors, such as attitudes (including beliefs about consequences), knowledge, intentions, perceived behavioral control (including beliefs about capabilities), skills, and perceived social norms, as outlined in the TDF [ 14 ]. These determinants are particularly significant as they represent core elements of many established behavioral theories and frameworks [ 36 ], making them crucial for understanding and driving clinical practice change among nurses.
Objective and research questions
The objective of this systematic review and meta-analysis was to assess the effects of healthcare professional-level implementation strategies, as defined in the EPOC Taxonomy [ 22 ], on nurses’ clinical practice and patient outcomes. We aimed to address the following questions:
What are the effects of implementation strategies on compliance with desired clinical practice in nurses (primary outcome) and patient outcomes (secondary outcome)?
What are the effects of implementation strategies on six key determinants of nurses’ behavior in clinical practice, including attitudes, intentions, knowledge, perceived behavioral control, perceived social norms, and skills (secondary outcomes)?
What are the effects of multifaceted implementation strategies compared to single implementation strategies on compliance with desired clinical practice in nurses and patient outcomes?
This systematic review and meta-analysis was conducted based on the Cochrane Handbook for Systematic Reviews of Interventions [ 37 ] and is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement (see Additional file 1) [ 38 ].
Protocol and registration
The protocol was registered at the International Prospective Register of Systematic Reviews on 5/01/19 (PROSPERO CRD42019130446) and can be found online [ 39 ]. No changes have been made to the review methods since the protocol’s registration.
Search strategy and eligibility criteria
A search strategy was developed in collaboration with a Research Librarian using controlled vocabulary (e.g., MeSH terms) and keywords relating to implementation strategies, nurses, and study designs. Searches were undertaken in CINAHL, EMBASE, ERIC, PsycINFO, PubMed and Web of Science for literature published between database inception until February 26, 2023 (see Additional file 2). Other sources searched to identify additional relevant citations included the reference lists of included studies and relevant systematic reviews found through the Cochrane Database of Systematic Reviews and Google Scholar.
We included studies conducted with all types of nurses (e.g., registered nurses, nurse practitioners, clinical nurse specialists, licensed practical nurses) across any clinical setting. Studies were excluded if more than 10% of the sample consisted of other healthcare professionals or if results specific to nurses were not reported. Studies focusing on nursing students were excluded. Implementation strategies were defined as methods or techniques to promote the initial adoption and sustained use of evidence-based interventions, practices and programs [ 22 ]. Eligible studies were required to include at least one of the 19 healthcare professional-level implementation strategies outlined in the EPOC Taxonomy (see Table 1 ) [ 22 ]. Studies of financial interventions, patient-oriented organizational interventions, structural organizational interventions, and regulatory interventions were considered out of scope. The review allowed for studies with all types of comparators or usual care. Studies had to report either an objective measure of nurses’ practice, such as clinical interventions reported in patients' medical files or the number of tests ordered, or a subjective measure, such as self-reported performance of clinical interventions. Studies which focused solely on determinants of nurses’ practice were excluded. In terms of study designs, the review included all types of randomized studies including randomized controlled trials (RCTs), cluster randomized trials (CRTs) and stepped wedge CRTs. We also included non-randomized controlled studies (NRCS). Cross-sectional studies, observational studies, and case reports were excluded. Only published peer-reviewed articles were included to allow for detailed review of intervention components; conference abstracts, dissertations and theses were excluded.
Selection of studies
Identified records were imported into EndNote X8 [ 40 ] and duplicates were removed. The remaining records were imported into the Covidence software [ 41 ] for screening where additional duplicates were removed automatically. Titles, abstracts, and full texts were screened in duplicate in Covidence for eligibility by two reviewers with conflicts resolved through discussion or moderation of a third reviewer.
Data extraction
All data were extracted in duplicate in Covidence by two reviewers with conflicts resolved through discussion or moderation of a third reviewer. Data were extracted for study, participant, and intervention characteristics (e.g., strategies in each study arm according to the EPOC Taxonomy), as well as our primary and secondary outcomes, into a pre-piloted and standardized data extraction form (Microsoft Excel for Office 365). All corresponding study authors were contacted by email to clarify study details and to obtain additional study characteristics and results data. Two reminder emails were sent to authors who did not respond to the initial request.

Assessment of risk of bias
For RCTs, risk of bias was assessed with the Cochrane Risk of Bias 2 (RoB 2) tool for randomized trials [ 42 ]. For CRTs, risk of bias was assessed with the Cochrane RoB 2 tool for CRTs [ 42 ]. For NRCS, risk of bias was assessed with the Risk Of Bias in Non-randomized Studies-of Interventions (ROBINS-I) tool [ 43 ]. If a single study reported multiple outcomes relevant to the review, risk of bias was assessed for each outcome. RCTs were ranked as having low risk, some concerns, or high risk of bias across five domains, and the overall risk of bias was derived. CRTs were ranked as having low risk, some concerns, or high risk of bias across six domains, and the overall risk of bias was derived. NRCS were ranked as having a low, moderate, serious, or critical risk of bias across seven domains, and the overall risk of bias was derived. Two reviewers assessed risk of bias independently, with conflicts resolved through discussion.
Measures of intervention effect
All continuous and dichotomous outcomes related to clinical practice were expressed in terms of compliance with the desired practice or process of care completed by a nurse. In cases where studies reported both dichotomous and continuous measures for the same targeted behavior, we extracted and conducted separate analyses for each type of measure. We prioritized the extraction of individual clinical practice measures over summary or composite measures whenever the former were available.
In situations where the intervention aimed to reduce a targeted behavior to align more closely with established guidelines, we inverted the outcome data for both continuous and dichotomous measures to ensure a consistent direction of effect and interpretation across studies. When a study measured multiple clinical practice outcomes, we selected the outcome identified as the primary outcome by the study authors. If the primary outcome was not specified, we extracted the first outcome listed in the results section.
Additional continuous and dichotomous outcomes extracted, where available, included nurses’ attitudes (encompassing beliefs about consequences), defined broadly as emotional and evaluative responses to a clinical behavior; intention, defined as readiness to perform a clinical behavior; knowledge, defined as the awareness and understanding of specific facts, techniques, or processes that affect the clinical behavior; perceived behavioral control (encompassing beliefs about capabilities, self-efficacy), defined broadly as nurses’ perception of their ability to perform a clinical behavior; perceived social norms (encompassing social influences), defined broadly as nurses’ perception about the normative expectations of others regarding a clinical behavior; and skills, defined as the practical abilities to perform a clinical behavior. We also extracted continuous and dichotomous outcomes related to patient health, defined as patient health status, reduction in symptoms, and other health improvements reasonably attributable to the nursing care provided.
For outcomes assessed at multiple time points, we selected data from the longest follow-up period. In the case of cross-over studies, we used data from the first period only due to the risk of carryover effects.
Data analysis
Where data were available, we performed DerSimonian and Laird random-effects meta-analyses of the primary (clinical practice) or secondary outcomes (patient outcomes; nurses’ attitudes, intentions, knowledge, perceived control, perceived social norms, and skills) across various intervention categorizations outlined in Table 1 . We synthesized the pooled estimate of studies in which the implementation strategy was present vs. not present (e.g., audit and feedback in the intervention arm [IA] vs. no active intervention or another implementation strategy in the control arm [CA]). We also synthesized the pooled estimate of studies comparing directly a multifaceted strategy to a single strategy.
For dichotomous outcomes, a pooled odds ratio (OR) with a 95% confidence interval (CI) was calculated in Review Manager Web (RevMan Web) Version 7.7.0 [ 44 ] using the proportion of people with each outcome of interest. A fixed continuity correction of 0.5 was applied where there was a 0 cell in calculating ORs. For continuous outcomes, we calculated the standardized mean difference (SMD) by using the difference between the post-test means, divided by the pooled standard deviation (SD) in RevMan Web since studies used a wide range of outcome measures for diverse constructs and targeted behaviors. Missing SDs were obtained, when possible, by using CIs or standard errors in calculations detailed in the Cochrane Handbook [ 37 ]. For the CRTs included, we conducted analyses adjusting for clustering with the design effect when possible. The design effect was calculated using the intracluster correlation coefficient (ICC), the number of clusters and the average sample size of each cluster [ 37 ]. Stepped-wedge CRTs were only included for descriptive purposes and were not used in the analysis due to the inability to adjust for time effects. For studies with multiple intervention groups, we included each pairwise comparison relevant to this review separately, but with shared control groups divided out approximately evenly among the comparisons [ 37 ]. Missing data regarding study and intervention characteristics, as well as results, were not imputed. Missing data regarding ICCs were imputed based on the median ICC observed in the extracted data. Two-sided p values of less than 0.05 were deemed to be statistically significant.
In addition to the quantitative analyses, we conducted a narrative synthesis to summarize and interpret the findings from studies that could not be included in the meta-analysis due to missing data, the nature of the outcome, or the nature of the comparison. As recommended in the Cochrane Handbook [ 37 ], we used the direct of the effects to synthesize findings narratively.
Tables were created to present the characteristics of included studies, the effects of implementation strategies on both primary and secondary outcomes, and the effects of implementation strategies on clinical practice outcomes across strata for the primary comparison.
Risk of bias judgments for each extracted outcome were summarized by domain using RoB 2 and ROBINS-I, and presented through risk of bias graphs and summaries with the risk of bias visualization tool (robvis) [ 45 ].
Subgroup analysis, investigation of heterogeneity and non-reporting bias
We assessed heterogeneity across studies using the I 2 statistic ( I 2 of less than 25% = low heterogeneity; I 2 25–75% = moderate heterogeneity; I 2 of more than 75% = high heterogeneity) and by visually examining forest plots to explore the range of effect sizes for comparisons of interest. We investigated heterogeneity by stratifying the meta-analysis for our first comparison (i.e., any implementation strategy versus no active intervention) based on the study design, the study setting, the targeted clinical behavior in nurses, and the intervention (i.e., implementation strategy group). We assessed non-reporting bias with funnel plots for our primary outcome.
Sensitivity analysis
We conducted a sensitivity analysis by excluding studies with unclear to high risk of bias to assess their potential impact on study outcomes.
Assessment of the certainty of the evidence and summary of findings
Two reviewers assessed the quality of evidence independently for each outcome using the five domains of the Grading of Recommendations Assessment, Development, and Evaluation (GRADE) approach [ 46 ] in the GRADEpro GDT software [ 47 ]: risk of bias, inconsistency, indirectness, imprecision, and publication bias. A third reviewer helped resolve any discrepancies in the assessments. Risk of bias was assessed by the percentage of studies evaluated as low risk of bias in a given comparison (not serious > 50% studies, serious 21–50%, very serious ≤ 20%). The certainty of evidence was rated for each outcome as “very low,” “low,” “moderate,” or “high.” A table was created to present an overview of effects and the certainty of evidence for clinical practice and patient outcomes, and summary of findings tables were created for all comparisons and outcomes.
Results of the search and included studies
We identified 30,134 records from bibliographical databases and 39 from other sources, resulting in 21,602 unique records (see Fig. 1 ). Out of 837 records assessed for eligibility, 204 studies were included: 152 randomized studies and 52 controlled, non-randomized studies, enrolling 36,544 nurses (reported in 161 studies) and 340,320 patients (reported in 88 studies). All corresponding authors were contacted, and a total of 78 authors (38%) responded to requests for additional data. Out of the 204 studies included in the review, 160 contributed data to the meta-analyses for our primary outcome (compliance with desired clinical practice) and 44 were synthesized narratively.
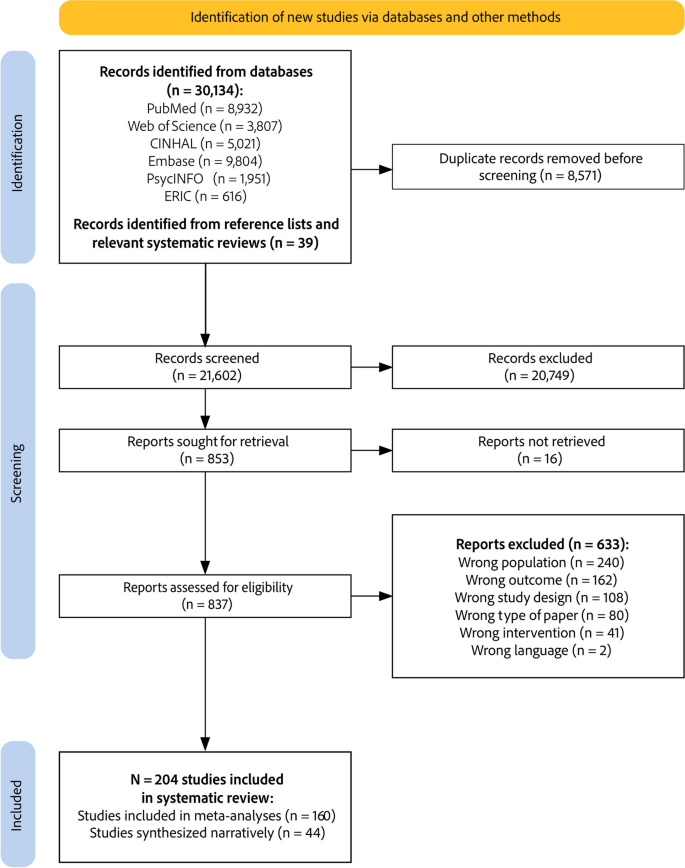
PRISMA study flow diagram
Characteristics of included studies
A summary of the characteristics of included studies is presented in Table 2 . The majority were randomized studies (152 studies, 75%), including 96 CRTs (47%), 51 RCTs (25%), and 5 stepped-wedge CRTs (2%), involving a total of 30,473 nurses and 323,986 patients. Non-randomized studies accounted for 52 studies (25%), including 38 non-randomized controlled trials (19%), 13 non-randomized cluster-controlled trials (6%), and 1 controlled time series study (< 1%), involving 6,071 nurses and 16,334 patients. Most studies were conducted in hospital settings, particularly inpatient or emergency departments (139 studies; 68%). Primary care or general practice settings comprised 25 studies (12%), and nursing homes accounted for 21 studies (10%). Other settings included community health centers, homecare, hospital outpatient settings, public health units and skilled nursing facilities. In terms of country income status, most studies were conducted in high-income countries (160 studies, 78%), followed by upper-middle-income countries (37 studies, 18%), and a small number in lower-middle-income (7 studies, 3%) and low-income countries (1 study, < 1%). The studies targeted various clinical behaviors, with the most common focus on multiple behaviors (48 studies, 24%). Common behaviors included: providing counseling and advice (29 studies, 14%), infection prevention and control practices (26 studies, 13%), assessing and diagnosing illness (26 studies, 13%), administering medication (14 studies, 7%), documenting care (10 studies, 5%), and coordinating care (10 studies, 5%). Behaviors targeted in less than 5% of studies included testing and screening, managing physical restraints, managing symptoms, managing care equipment, prescribing, vaccinating, and reporting clinical incidents. Additional file 3 presents the characteristics of all included studies. Additional file 4 presents the excluded articles at full text assessment stage and reasons for exclusion.
Risk of bias across included studies
We summarized the decisions regarding individual domains within the Cochrane RoB 2 tool and ROBINS-I in the risk of bias summary (see Fig. 2 ). Overall, for CRTs, the risk of bias for all outcome assessments ( N = 227 from 96 CRTs and 5 stepped-wedge CRTs) was distributed as follows: 50% were assessed as low risk, 29% had some concerns, and 21% were considered high risk. For RCTs ( N = 127 outcome assessments across 51 RCTs), 50% of the assessments were categorized as having some concerns, 28% as high risk, and 22% as low risk. For NRCS ( N = 85 outcome assessments across 52 NRCS), 55% were considered to have a critical risk, 25% a serious risk, 18% a moderate risk and 2% a low risk. The full risk of bias assessment for each outcome, for RCTs, CRTs and NCRS is presented in Additional file 5.

a Summary of risk of bias for cluster randomized trials. b Summary of risk of bias for randomized controlled trials. c Summary of risk of bias for non-randomized controlled studies
Use of implementation strategies across included studies
As illustrated in the panel a of Fig. 3 , among the implementation strategies employed in at least 10% of the studies, educational meetings were the most common (intervention arms [IAs] N = 155; control arms [CAs] N = 29), followed by educational materials (IAs N = 145; CAs N = 22), clinical practice guidelines (IAs N = 64; CAs N = 13), reminders (IAs N = 43; CAs N = 3), audit and feedback (IAs N = 38; CAs N = 1), educational outreach (IAs N = 32; CAs N = 1), tailored interventions (IAs N = 26; CAs N = 2), and local opinion leaders (IAs N = 24; CAs N = 3). Strategies employed in less than 10% of studies included patient-mediated interventions, local consensus processes, monitoring the performance of delivery of healthcare, clinical incident reporting, interprofessional education, communities of practice, managerial supervision, routine patient-reported outcome measures, educational games, and continuous quality improvement. No intervention used public release of performance data.
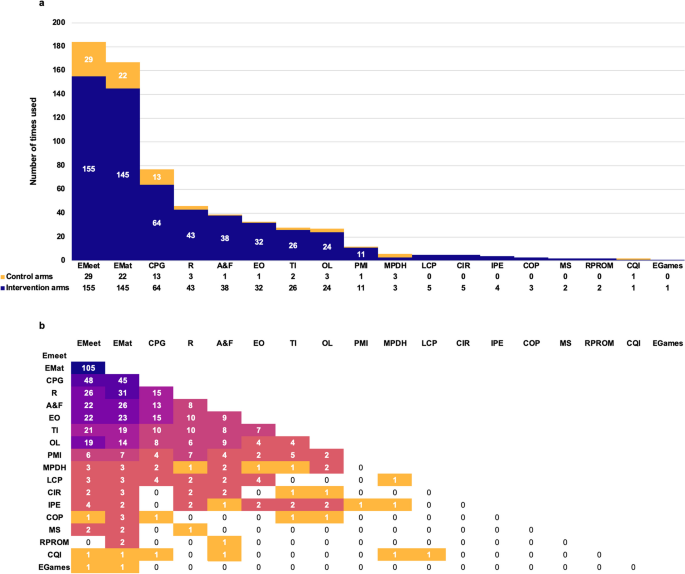
a Frequency of use of each implementation strategy across intervention and control arms. b Frequency of combinations of implementation strategies in interventions assessed in included studies. EMeet = educational meetings, EMat = educational materials, CPG = clinical practice guidelines, R = reminders, A&F = audit and feedback, EO = educational outreach, TI = tailored interventions, OL = local opinion leaders, PMI = patient-mediated interventions, MPDH = monitoring the performance of delivery of healthcare, LCP = local consensus processes, CIR = clinical incident reporting, IPE = interprofessional education, COP = communities of practice, MS = managerial supervision, RPROM = routine patient-reported outcome measures, CQI = continuous quality improvement, EGames = educational games
As illustrated in the panel b of Fig. 3 , implementation strategies almost always included some form of individual clinician education (including educational materials, educational outreach, and clinical practice guidelines) and/or group clinician education (including communities of practice, educational meetings, and interprofessional education) combined with reminders, audit and feedback, local opinion leaders, and tailored interventions. Additional file 3 presents the implementation strategies used across study arms.
Effects of implementation strategies
Effects of implementation strategies as a whole compared to no active intervention.
In comparison with no active intervention, implementation strategies as a whole had significant positive effects on continuous clinical practice outcomes (76 assessments; SMD 0.94, 95% CI 0.72–1.15; I 2 = 95%; see Fig. 4 ), and dichotomous clinical practice outcomes (60 assessments; OR 2.11, 95% CI 1.70–2.62; I 2 = 95%; see Fig. 5 ). Statistically significant positive effects were also observed on nurses’ attitudes (30 assessments; SMD 0.59, 95% CI 0.23–0.95; I 2 = 92%), knowledge (37 assessments; SMD 1.16, 95% CI 0.82–1.49; I 2 = 91%), perceived behavioral control (19 assessments; SMD 0.74, 95% CI 0.35–1.13; I 2 = 91%), and skills (10 assessments; SMD 0.97, 95% CI 0.42–1.52; I 2 = 87%). No significant effects were observed on continuous patient outcomes (10 assessments; SMD 0.23, 95% CI -0.01–0.47; I 2 = 87%) and dichotomous patient outcomes (12 assessments; OR 1.46, 95% CI 0.96–2.22; I 2 = 84%). Statistical heterogeneity was high in all analyses. All forest plots are presented in Additional file 6. The clinical practice outcomes included in meta-analyses across all comparisons are presented in Additional file 7.
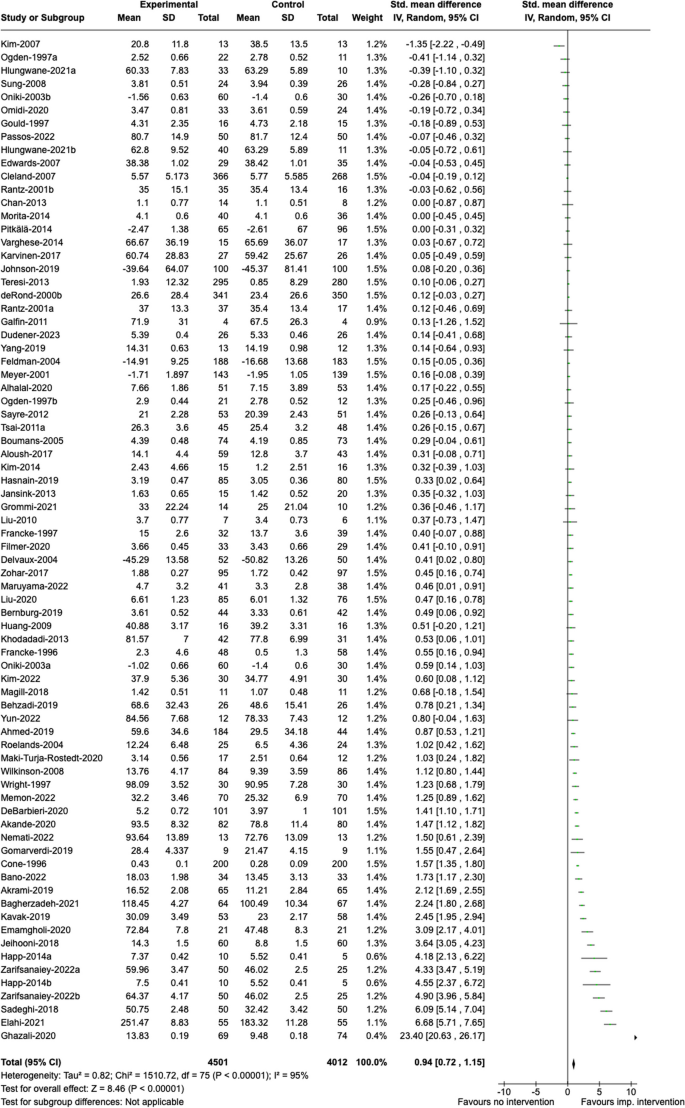
Effects of implementation strategies on continuous clinical practice outcomes, compared with no active intervention
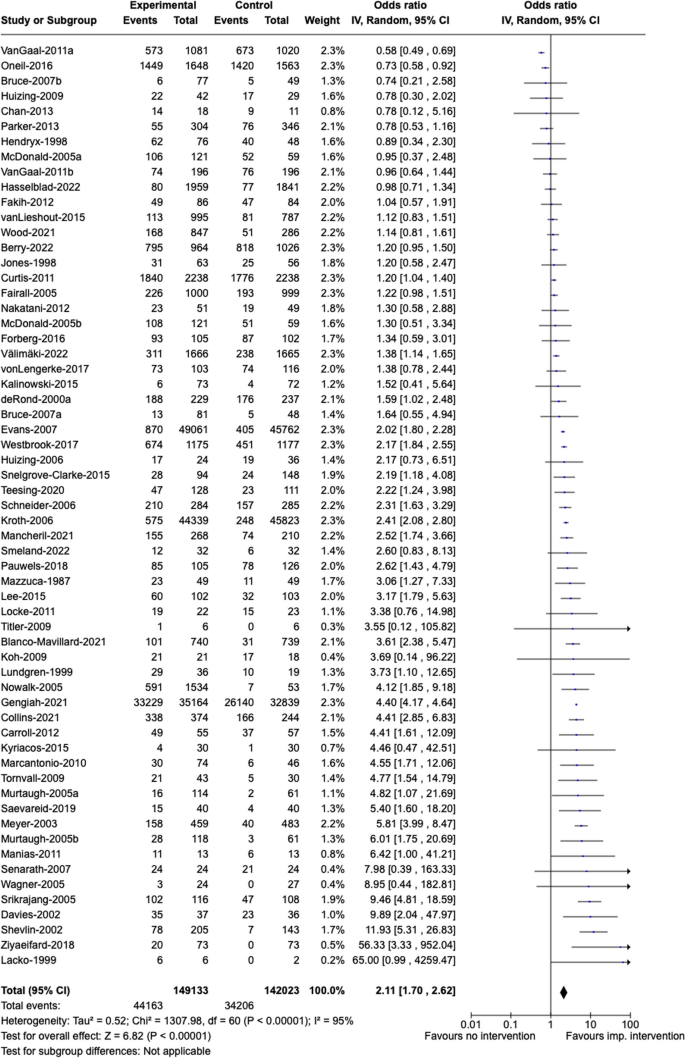
Effects of implementation strategies on dichotomous clinical practice outcomes, compared with no active intervention
Table 3 presents subgroup analyses of the estimated SMDs for continuous outcomes and the estimated ORs for dichotomous outcomes to illuminate the variance in effects attributed to study design, study setting, and clinical behavior targeted for change. Minimal differences in effects were noted across these strata. Though, primary care/general practice for continuous clinical practice outcomes decreased and was no longer significant.
Effects of specific implementation strategies on primary and secondary outcomes
Table 4 displays effects of the implementation strategy subgroups by the primary outcome. Dichotomous clinical practice outcomes are positively affected (i.e., more likely to align with desired practice) by group clinician education, individual clinician education, reminders, patient-mediated interventions, tailored interventions, and opinion leaders. Continuous clinical practice outcomes are positively affected by group clinician education, individual clinician education, and tailored interventions. Across all implementation strategy subgroups, group clinician education, individual clinician education and tailored interventions had statistically significant effects on patient outcomes. These results may be influenced by heterogeneity and the lack of control over co-existing strategies within these subgroup analyses, likely leading to an inflation of the effects of individual strategies.
Table 5 displays effects of the implementation strategy subgroups by secondary outcomes. Attitude (continuous) was positively influenced by group clinician education, individual clinician education, audit and feedback, and tailored interventions. Attitude (dichotomous) was positively influenced by group clinician education and individual clinician education. Knowledge was positively influenced by group clinician education, individual clinician education, and tailored interventions. Perceived behavioral control was positively influenced by group clinician education, individual clinician education, and reminders. Skills were positively influenced by group clinician education and individual clinician education. Perceived social norms were positively influenced by group clinician education.
Effects of multifaceted implementation strategies compared to single implementation strategy
In studies comparing a multifaceted implementation strategy (combining two or more implementation strategies) with a single type of implementation strategy, multifaceted strategies had small, non statistically significant effects on continuous clinical practice outcomes (12 assessments; SMD 0.23, 95% CI -0.01–0.46; I 2 = 77%; see panel a of Fig. 6 ), dichotomous clinical practice outcomes (20 assessments; OR 1.35, 95% CI 0.76–2.40; I 2 = 91%; panel b of Fig. 6 ), and dichotomous patient outcomes (5 assessments; OR 1.30, 95% CI 0.89–1.90; I 2 = 0%) (see Additional file 6).
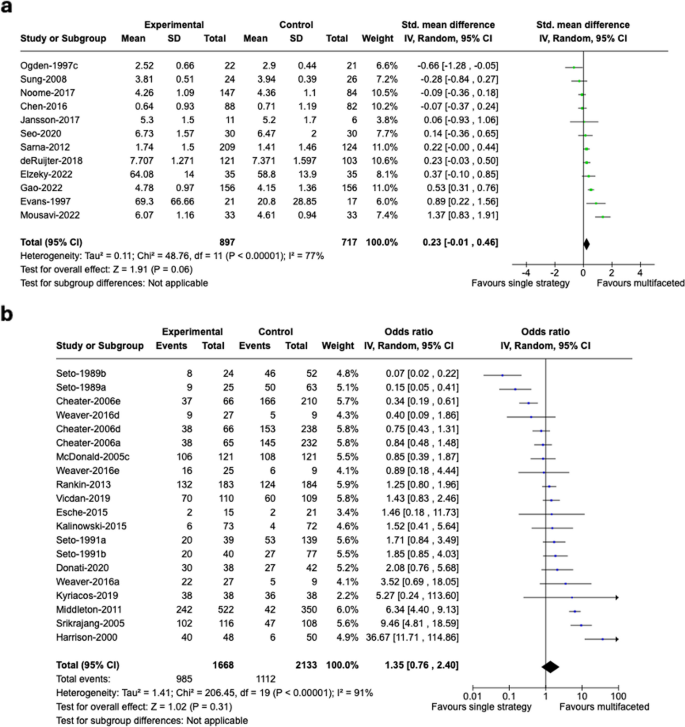
Effects of multifaceted vs. single strategies on continuous ( a ) and dichotomous ( b ) clinical practice outcomes
Effects of implementation strategies in included studies not ineligible for meta-analysis
After contacting all study authors, 44 studies were not included in meta-analyses for our primary outcome due to missing data ( n = 27) [ 48 , 49 , 50 , 51 , 52 , 53 , 54 , 55 , 56 , 57 , 58 , 59 , 60 , 61 , 62 , 63 , 64 , 65 , 66 , 67 , 68 , 69 , 70 , 71 , 72 , 73 , 74 ], comparisons that were not relevant to our analyses (e.g., comparing two groups receiving the same type of implementation strategy with design variations) ( n = 14) [ 75 , 76 , 77 , 78 , 79 , 80 , 81 , 82 , 83 , 84 , 85 , 86 , 87 , 88 ], or expressing their outcomes as rates rather than in a compatible format ( n = 3) [ 89 , 90 , 91 ].
Of these studies, 25 focused solely on educational strategies, with 22 showing more favorable outcomes in the experimental groups. Kaner et al. [ 78 ] demonstrated that educational outreach increased brief alcohol interventions compared to clinical practice guidelines. Educational meetings (EMeet), often supplemented with educational materials (EMat) and/or clinical practice guidelines (CPG), led to improvements across various areas: blood glucose monitoring (O’Neill et al.: EMeet), [ 63 ] communication (Antonini et al.: EMeet), [ 48 ] diabetes management (Lim et al.: EMeet + EMat), [ 59 ] endotracheal suctioning practices (Day et al.: CPG + EMeet), [ 52 ] nursing documentation and care planning (Müller-Staub et al.: EMeet; Brady et al.: EMeet), [ 49 , 81 ] use of physical restraints (Chang et al.: EMeet), [ 51 ] counseling (Tsai et al.: EMeet; Woodcock et al.: EMeet), [ 72 , 86 ] and symptom management (Hessig et al.: EMat + EMeet; Michaels et al.: CPG + EMat + EMeet). [ 55 , 61 ] Magnan et al. [ 80 ] used educational materials alone to improve physical examination. Nine studies evaluated technology-enhanced educational strategies. Carrico et al. [ 87 ] reported that biosimulated visual demonstration of particulate transmission resulted in increased personal protective equipment use. Jansson et al. [ 84 , 92 ], through two studies, demonstrated adding feedback and debriefing to simulation-focused educational meetings, improved nurses' adherence to evidence-based guidelines for mechanical ventilation. Rutherford-Hemming et al. [ 82 ] found higher levels of evidence-based performance of neurological examinations in simulation-based education compared to a self-study module. Wang et al. [ 83 ] found improved application of counseling following the additional of simulation to educational meetings and materials. Wang et al. reported the effects of game-based learning on hand hygiene practices. [ 85 ] Kinsman et al. [ 88 ], Lau et al. [ 79 ], and Van de Steeg et al. [ 70 ] found e-learning programs improved physical examination, medication administration, and delirium care. Hammersley et al. [ 53 ], Seeley et al. [ 68 ], and Segal et al. [ 69 ] found no benefits from educational strategies.
Four out of five studies using audit and feedback alone were inconclusive. Charrier et al. [ 76 ] found that audit and feedback and the presence of facilitators, compared with self-monitoring, improved compliance to protocols for pressure lesions and the management of catheters. Bittner et al. [ 75 ], Hutchinson et al. [ 91 ], Noordman et al. [ 62 ], and Rothschild et al. [ 66 ] found no effects of audit and feedback on hand hygiene, history-taking, the reporting of medication errors, and medication errors.
Studies using multifaceted implementation strategies including other strategies than education compared to no active intervention were often successful, with 9 out of 10 showing positive results. Brennan et al. [ 50 ] evaluated a tailored intervention using the CAM-ICU guideline, which increased delirium screenings and led to a decrease in delirium rates. Chambers et al. [ 89 ] and Fabre et al. [ 90 ] found that a multifaceted implementation strategy reduced nurse-led urine culturing. Hödl et al. [ 56 ] improved urinary incontinence equipment management using educational outreach, materials, guidelines, and reminders. Documentation improved by 43% in the multi-faceted group, while the control group saw a 15% decrease after 2 weeks. Lin et al. [ 60 ] found that a multifaceted strategy (audit and feedback, tailored intervention, educational meetings, and materials) improved the use of relaxation techniques in surgical nurses in Taipei. Morita et al. [ 73 ] found improved palliative care practices following a multifaceted strategy involving tailoring and education. Reynolds et al. [ 65 ] assessed a multifaceted strategy (educational outreach, educational materials, audit and feedback) to improve compliance with chlorhexidine gluconate bathing documentation and reduce central line-associated bloodstream infections. While CHG bathing compliance increased significantly by 6.97%, the 27.4% decrease in CLABSI rates was not significant. Schondelmeyer et al. [ 67 ] reported that education (meetings, clinical practice guidelines, outreach) with audit and feedback reduced guideline-discordant continuous pulse oximetry use by 30% in pediatric nurses in the USA. Wald et al. [ 74 ] also found effects of audit and feedback on the uptake of catheter-associated urinary tract infection prevention measures. One study of a multifaceted implementation strategy had inconclusive results. Happ et al. [ 93 ] evaluated a web-based training with local opinion leaders to reduce ICU adverse events, finding no significant changes in physical restraint use.
Four studies specifically compared the effects of multifaceted versus single-component strategies, with all favoring multifaceted strategies. Hong et al. [ 57 ] found higher urinary catheter care practice implementation using local opinion leaders with educational meetings, than either component alone. Johnston et al. [ 58 ] used audit and feedback, local opinion leaders, and educational materials compared to only monitoring healthcare delivery on the documentation of pain assessment in Canadian patients. Pagaiya et al. [ 64 ] compared a multifaceted strategy to guidelines alone for reducing antibiotic prescriptions in Thailand. Walsh et al. [ 71 ] found that web-based education with process feedback significantly reduced oversedation in ICU patients in the UK, more than other education methods.
Sensitivity analyses
We conducted sensitivity analyses to exclude studies assessed as being at overall unclear or high risk of bias, as presented in Additional file 8. Effect measures tended to decrease with the removal of high risk of bias studies, though most remained statistically significant. In rare instances, the effect sizes increased, such as with continuous clinical practice outcomes for multifaceted interventions compared to single strategy interventions. Heterogeneity remained high in most analyses.
Non-reporting bias
Funnel plots indicated some evidence for non-reporting bias in dichotomous clinical practice outcomes (any vs no implementation strategies comparison), continuous clinical practice outcomes (individual clinician education comparison), and continuous clinical practice outcomes (group clinician education comparison) (Additional file 9). These studies tend to be heavily concentrated to the upper left of the triangle suggesting that the effect measure could be underestimated for the intervention. We did not find clear evidence for non-reporting bias for other outcomes.
Certainty of the evidence
Table 6 provides an overview of the impact of various implementation strategies compared with different or no active interventions for improving compliance with desired clinical practice and patient outcomes. The table presents both quantitative findings from meta-analyses and narrative findings from studies not included in the meta-analyses. It also includes the certainty of evidence (GRADE) for each type of intervention and outcome, offering a comprehensive view of how different strategies influence clinical practice and patient care. Detailed summary of findings tables are presented in Additional file 10.
This systematic review examined the effects of healthcare professional-level implementation strategies on nursing practice and patient outcomes across 204 studies. Overwhelmingly, the implementation strategies described were multi-component, primarily involving individual and group education (e.g., educational meetings, educational materials, clinical practice guidelines, communities of practice, interprofessional education) combined with reminders, audit and feedback, local opinion leaders, and tailored interventions. In a quarter of the included studies, implementation strategies targeted multiple clinical behaviors for change, such as providing counseling and advice, practicing hand hygiene, assessing and diagnosing illness, administrating medication and documenting care. Meta-analyses of 160 studies and narrative synthesis of 44 studies not eligible for meta-analysis revealed that both single and multifaceted implementation strategies have positive effects on clinical practice outcomes, with important variability across strategies. Statistically significant and practically meaningful positive effects were also observed for secondary outcomes including nurses’ attitudes, knowledge, perceived behavioral control and skills for strategies consisting of individual or group education, reminders, and tailored interventions. Effects on patient outcomes were observed for group and individual education, as well as tailored interventions.
Our findings are consistent with previous reviews of implementation strategies, demonstrating the positive effects of group and individual education, reminders, patient-mediated interventions, and the involvement of opinion leaders on clinical practice outcomes. A systematic review by Spoon et al. [ 35 ] similarly identified a broad spectrum of implementation strategies that positively influenced guideline adherence among nurses and improved patient-reported nursing outcomes. Likewise, Cassidy et al. [ 34 ] found that combining educational meetings with other strategies, such as educational materials and opinion leaders, effectively supported guideline-concordant nursing care. Forsetlund et al. [ 16 ] associated educational meetings with likely improvements in professional practice and patient outcomes, while Giguère et al [ 27 ] observed that printed educational materials, when used alone and compared to no intervention, might improve slightly healthcare professionals' practices and patient health outcomes. Additionally, Flodgren et al. [ 26 ] reported that opinion leaders, whether alone or in combination with other interventions, can promote evidence-based practice, though their effectiveness varies across studies. However, despite its widespread use, audit and feedback have shown mixed results. A systematic review by Ivers et al. [ 94 ] indicated small improvements in professional practice among physicians but provided limited evidence of effectiveness among nurses. In our meta-analyses, strategies including audit and feedback did not achieve statistically significant impacts on clinical practice outcomes (a sensitivity analysis excluding high-risk-of-bias studies showed a statistically significant effect, but only in two studies). This may be due to limited statistical power, heterogeneity, or limitations of this strategy in inducing practice change among nurses. Notably, while 9 out of 14 studies of strategies including audit and feedback synthesized narratively favored the experimental group in terms of clinical practice outcomes, 8 of these studies involved multifaceted strategies.
Additionally, our review highlights the underuse of many implementation strategies. Ten out of 19 EPOC strategies examined were used in less than 5% of included studies. This suggests a need for further exploration and integration of the full range of EPOC strategies to potentially enhance nursing practice and patient outcomes. Furthermore, there is a need to consider additional taxonomies of implementation strategies, such as the Expert Recommendations for Implementing Change (ERIC) Taxonomy, which outlines 73 unique strategies across 9 clusters [ 20 ]. Designing and evaluating multifaceted strategies using a broader range of implementation strategies could help address the gaps in current implementation research and practice. While our exploration of the effects of implementation strategies on determinants of nurses’ behavior is novel and provides insights on the effectiveness of educational strategies on attitudes, intentions, knowledge, perceived behavioral control, perceived social norms, and skills, further research could benefit from examining outcomes through the lens of the TDF [ 14 ] and the Capability, Opportunity, Motivation and Behavior (COM-B) Model [ 95 ], as these frameworks allow for a deeper understanding of the determinants of behavior change.
Our findings contribute to the ongoing discussion about the effectiveness of multifaceted versus single component implementation strategies. An overview of reviews by Squires et al. [ 96 ] found no strong evidence that multifaceted strategies significantly improve outcomes compared to single interventions. A more recent overview of reviews by Boaz et al. [ 25 ], without quantitative analyses, concluded that the effectiveness of multifaceted strategies compared to single strategies is nuanced and context-dependent. The authors discussed that while multifaceted strategies appear to be more likely to generate positive results than single strategies, the evidence varies, and the impact on patient outcomes is often limited. In our review, while quantitative findings suggest a small, non-statistically significant effect of multifaceted versus single strategies on clinical practice, the narrative synthesis of studies with outcomes ineligible for meta-analysis shows favorable outcomes in all four studies using multifaceted strategies compared to single strategies. These multifaceted strategies typically combined elements such as educational outreach, audit and feedback, tailored interventions, and the use of local opinion leaders. This might indicate that multifaceted strategies can enhance the uptake of evidence-based practice among nurses more effectively than single strategies. However, the translation of these improvements to better patient outcomes is uncertain. Tailoring strategies and ensuring organizational capacity to support research utilization, as emphasized by Boaz et al. [ 25 ], are crucial. Our analyses showed that tailored strategies based on contextual assessments of implementation barriers and enablers had significant effects on professional outcomes and patient outcomes. This suggests that strategies customized to address specific barriers and facilitators within a particular context, echoing a previous systematic review by Baker et al., [ 97 ] may be more effective in driving improvements in patient care.
The analysis reveals that while implementation strategies can improve clinical practice outcomes among nurses, their impact on patient outcomes is modest. This observation aligns with broader research, which suggests that while nurses play a crucial role in healthcare delivery, the direct translation of their practice improvements into measurable patient benefits is influenced by a multitude of factors. The pathway from practice changes to patient outcomes is complex, shaped by organizational culture, patient engagement, and broader systemic issues within healthcare settings [ 16 , 17 , 25 ]. Considering the role of these factors and the influence of other healthcare professionals, nurses can have a nuanced and often indirect influence on patient outcomes within the larger healthcare system [ 6 ]. However, several outcomes directly affected by nursing practice were not extracted in the context of this review, such as length of stay, readmissions and patient satisfaction [ 98 ]. Additionally, we extracted the longest follow-up measurements for all outcomes, which may have diminished the observed effects. Consequently, it is important to interpret these overall averages and findings with caution, given the effects of strategies may vary significantly depending on the context, target behaviors, actors, outcomes and specific populations involved.
The predominance of studies (190 studies) from high-income countries highlights a critical gap in the literature regarding the effectiveness of implementation strategies on nursing practice in low- and middle-income countries (LMIC). A recent review using the ERIC Taxonomy suggests that many implementation strategies can be applied to LMIC contexts [ 99 ]. However, out of 60 studies in this review, a minority of studies employed randomized trials or high-quality quasi-experimental designs with controls, and just one study evaluated implementation strategy effectiveness [ 99 ]. Future research should focus on exploring the adaptation and evaluation of professional implementation strategies in diverse contexts to ensure global relevance and equity in healthcare improvements.
A key strength of this systematic review is its focus on nursing practice, improving comparability across studies. The inclusion of studies conducted with multiple types of healthcare providers in previous systematic reviews of implementation strategies constitutes an important source of heterogeneity. Additional strengths include the extraction of continuous and dichotomous clinical practice and patient outcomes, as well as a comprehensive range of determinants preceding clinical practice in nurses (e.g., social norms, attitudes, intentions), providing additional insights on the effects of implementation strategies. Other methodological strengths of the review include contacting all study authors systematically to obtain additional data, the use of the EPOC Taxonomy to guide data extraction and analysis of findings and the use of GRADE to assess the certainty of evidence and enhance the reliability of the review’s conclusions.
This review also has limitations. The presence of multiple co-interventions and varying study designs could confound the results, making it challenging to isolate the effect of specific implementation strategies. Some studies were judged to have a high risk of bias, potentially affecting the reliability of the findings, though sensitivity analyses were conducted to exclude these studies. Additionally, we could not abstract some important factors, such as organizational and contextual characteristics, and the effects of implementation strategies depend on engagement with the intervention, which was not measured or reported in many studies. We synthesized and described a very large, heterogeneous dataset, which we believed could not be meaningfully summarized effectively through a narrative approach alone. The meta-analyses demonstrated substantial heterogeneity for most analyses ( I 2 often above 75%), indicating significant variability in the effect sizes across studies. This high heterogeneity can reduce the reliability of the pooled estimates and suggests that the effects of implementation strategies may differ substantially depending on the context and specific characteristics of each study. There was considerable variation in the measurement and reporting of clinical practice and patient outcomes across studies. This variation complicates the comparison and synthesis of results and may contribute to the observed heterogeneity. For these reasons, the findings from our quantitative analyses should be interpreted with caution given that they rely on heterogenous and moderate quality data, and as a quantitative aid to the narrative synthesis.
This comprehensive review offers several actionable recommendations and implications for healthcare systems. Implementation practitioners and healthcare organizations may consider adopting and investing in multifaceted, tailored, context-specific strategies that address local barriers and leverage facilitators for the successful implementation of evidence-based interventions in nursing practice. Furthermore, practitioners and organizations should also consider expanding the repertoire of strategies they employ, incorporating underutilized strategies listed in the EPOC Taxonomy such as local consensus processes, patient-mediated interventions, and continuous quality improvement, while exploring additional strategies outlined in the ERIC Taxonomy. Finally, there is need for ongoing monitoring and evaluation mechanisms to assess the long-term impact of implementation strategies on both clinical practice and patient outcomes.
Implementation strategies play a crucial role in enhancing evidence-based nursing practice and potentially improving patient outcomes. Future research should focus on exploring how different healthcare settings and contexts influence the effectiveness of implementation strategies; investigating the sustainability and long-term impact of strategies on both clinical practice and patient outcomes; evaluating the effectiveness of novel and underutilized implementation strategies; evaluating the effectiveness of implementation strategies in diverse healthcare systems (particularly in LMICs); and designing trials that more rigorously measure the direct impact of implementation strategies on patient outcomes.
Availability of data and materials
All data are included in this published article and its supplementary information files.
Abbreviations
Audit and feedback
Chlorhexidine gluconate
Central line-associated bloodstream infections
Confidence interval
Clinical incident reporting
Clinical practice guidelines
Communities of practice
Continuous quality improvement
Cluster randomized trial
Educational games
Educational materials
Educational meetings
Educational outreach
Effective Practice and Organisation of Care Group
Expert Recommendations for Implementing Change
Intensive care unit
Inter-professional education
Local consensus processes
Low and middle-income countries
Monitoring the performance of delivery of healthcare
Managerial supervision
Local opinion leaders
Patient-mediated interventions
Randomized control trial
Review Manager Web
Risk of Bias 2
Risk Of Bias in Non-randomized Studies-of Interventions
Routine patient-reported outcome measures
Standard deviation
Sustainable Development Goals
Standardized mean difference
Tailored interventions
World Health Organization. State of the world’s nursing 2020: investing in education, jobs and leadership. 2020.
Google Scholar
World Health Organization. Global strategic directions for nursing and midwifery 2021–2025. 2021.
United Nations. Transforming our world: the 2030 Agenda for Sustainable Development - Resolution adopted by the General Assembly on 25 September 2015. 2015.
Fields L, Perkiss S, Dean BA, Moroney T. Nursing and the Sustainable Development Goals: a scoping review. J Nurs Scholarsh. 2021;53(5):568–77. https://doi.org/10.1111/jnu.12675 .
Article PubMed Google Scholar
Laurant M, van der Biezen M, Wijers N, Watananirun K, Kontopantelis E, van Vught AJ. Nurses as substitutes for doctors in primary care. Cochrane Database Syst Rev. 2018;7(7):CD001271. https://doi.org/10.1002/14651858.CD001271.pub3 .
Coster S, Watkins M, Norman IJ. What is the impact of professional nursing on patients’ outcomes globally? An overview of research evidence. Int J Nurs Stud. 2018;78:76–83. https://doi.org/10.1016/j.ijnurstu.2017.10.009 .
Nundy S, Cooper LA, Mate KS. The Quintuple Aim for health care improvement: a new imperative to advance health equity. JAMA. 2022;327(6):521–2. https://doi.org/10.1001/jama.2021.25181 .
Stephenson J. Expand Nurses’ Scope of Practice, Strengthen Nursing Education to Advance Health Equity, Report Advises. JAMA Health Forum. 2021;2(5):e211527. https://doi.org/10.1001/jamahealthforum.2021.1527 .
Patey AM, Fontaine G, Francis JJ, McCleary N, Presseau J, Grimshaw JM. Healthcare professional behaviour: health impact, prevalence of evidence-based behaviours, correlates and interventions. Psychol Health. 2023;38(6):766–94. https://doi.org/10.1080/08870446.2022.2100887 .
Cheraghi R, Ebrahimi H, Kheibar N, Sahebihagh MH. Reasons for resistance to change in nursing: an integrative review. BMC Nurs. 2023;22(1):310. https://doi.org/10.1186/s12912-023-01460-0 .
Article PubMed PubMed Central Google Scholar
Godin G, Belanger-Gravel A, Eccles M, Grimshaw J. Healthcare professionals’ intentions and behaviours: a systematic review of studies based on social cognitive theories. Implement Sci. 2008;3:36. https://doi.org/10.1186/1748-5908-3-36 .
McArthur C, Bai Y, Hewston P, Giangregorio L, Straus S, Papaioannou A. Barriers and facilitators to implementing evidence-based guidelines in long-term care: a qualitative evidence synthesis. Implement Sci. 2021;16(1):70. https://doi.org/10.1186/s13012-021-01140-0 .
Shayan SJ, Kiwanuka F, Nakaye Z. Barriers associated with evidence-based practice among nurses in low- and middle-income countries: a systematic review. Worldviews Evid Based Nurs. 2019;16(1):12–20. https://doi.org/10.1111/wvn.12337 .
Cane J, O’Connor D, Michie S. Validation of the theoretical domains framework for use in behaviour change and implementation research. Implement Sci. 2012;7:37. https://doi.org/10.1186/1748-5908-7-37 .
Dakka FJ. Nurses barriers to evidence-based practice in palliative care: a systematic review. SAGE Open Nurs Jan-Dec. 2022;8:23779608221142956. https://doi.org/10.1177/23779608221142957 .
Article Google Scholar
Forsetlund L, O'Brien MA, Forsen L, et al. Continuing education meetings and workshops: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2021;(9) https://doi.org/10.1002/14651858.CD003030.pub3
Ivers N, Jamtvedt G, Flottorp S, et al. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2012;(6) https://doi.org/10.1002/14651858.CD000259.pub3
Santos WJ, Graham ID, Lalonde M, Demery Varin M, Squires JE. The effectiveness of champions in implementing innovations in health care: a systematic review. Implement Sci Commun. 2022;3(1):80. https://doi.org/10.1186/s43058-022-00315-0 .
Cahill LS, Carey LM, Lannin NA, et al. Implementation interventions to promote the uptake of evidence‐based practices in stroke rehabilitation. Cochrane Database Syst Rev. 2020;(10) https://doi.org/10.1002/14651858.CD012575.pub2
Powell BJ, Waltz TJ, Chinman MJ, et al. A refined compilation of implementation strategies: results from the Expert Recommendations for Implementing Change (ERIC) project. Implement Sci. 2015;10:21. https://doi.org/10.1186/s13012-015-0209-1 .
Proctor EK, Powell BJ, McMillen JC. Implementation strategies: recommendations for specifying and reporting. Implement Sci. 2013;8:139. https://doi.org/10.1186/1748-5908-8-139 .
Effective Practice and Organisation of Care (EPOC). EPOC Taxonomy. https://epoc.cochrane.org/epoc-taxonomy . Accessed 20 Sept 2024.
Hulscher MWM. Multifaceted Implementation Strategies. In: Wensing MGR, Grimshaw J, editors. Improving Patient Care: The Implementation of Change in Health Care. 3rd ed. 2020.
Suman A, Dikkers MF, Schaafsma FG, van Tulder MW, Anema JR. Effectiveness of multifaceted implementation strategies for the implementation of back and neck pain guidelines in health care: a systematic review. Implement Sci. 2016;11(1):126. https://doi.org/10.1186/s13012-016-0482-7 .
Boaz A, Baeza J, Fraser A, Persson E. ‘It depends’: what 86 systematic reviews tell us about what strategies to use to support the use of research in clinical practice. Implement Sci. 2024;19(1):15. https://doi.org/10.1186/s13012-024-01337-z .
Flodgren G, O’Brien MA, Parmelli E, Grimshaw JM. Local opinion leaders: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2019;6(6):CD000125. https://doi.org/10.1002/14651858.CD000125.pub5 .
Giguere A, Legare F, Grimshaw J, et al. Printed educational materials: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2020;10(10):CD004398. https://doi.org/10.1002/14651858.CD004398.pub3 .
Maheu-Cadotte MA, Cossette S, Dube V, et al. Efficacy of serious games in healthcare professions education: a systematic review and meta-analysis. Simul Healthc. 2021;16(3):199–212. https://doi.org/10.1097/SIH.0000000000000512 .
Fontaine G, Cossette S, Maheu-Cadotte MA, et al. Efficacy of adaptive e-learning for health professionals and students: a systematic review and meta-analysis. BMJ Open. 2019;9(8):e025252. https://doi.org/10.1136/bmjopen-2018-025252 .
Maheu-Cadotte M-A, Lapierre A, Fontaine G, Mailhot T, Lavoie P. Effect of simulation-based education on the preparedness of healthcare professionals for the COVID-19 Pandemic: a systematic review and meta-analysis. Sci Nurs Health Pract. 2021;4(1):1–21. https://doi.org/10.7202/1077986ar .
Brown A, Barnes C, Byaruhanga J, et al. Effectiveness of Technology-Enabled Knowledge Translation Strategies in Improving the Use of Research in Public Health: Systematic Review. J Med Internet Res. 2020;22(7):e17274. https://doi.org/10.2196/17274 .
De Angelis G, Davies B, King J, et al. Information and communication technologies for the dissemination of clinical practice guidelines to health professionals: a systematic review. JMIR Med Educ. 2016;2(2):e16. https://doi.org/10.2196/mededu.6288 .
Pantoja T, Grimshaw JM, Colomer N, Castanon C, Leniz Martelli J. Manually-generated reminders delivered on paper: effects on professional practice and patient outcomes. Cochrane Database Syst Rev. 2019;12(12):CD001174. https://doi.org/10.1002/14651858.CD001174.pub4 .
Cassidy CE, Harrison MB, Godfrey C, et al. Use and effects of implementation strategies for practice guidelines in nursing: a systematic review. Implement Sci. 2021;16(1):102. https://doi.org/10.1186/s13012-021-01165-5 .
Spoon D, Rietbergen T, Huis A, et al. Implementation strategies used to implement nursing guidelines in daily practice: a systematic review. Int J Nurs Stud. 2020;111:103748. https://doi.org/10.1016/j.ijnurstu.2020.103748 .
Michie S. ABC of behaviour change theories. London: Silverback Publishing; 2014.
Higgins JPT, Thomas J, Chandler J, et al. Cochrane handbook for systematic reviews of interventions. 2 ed. Oxford: Wiley Blackwell; 2019.
Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Syst Rev. 2021;10(1):1–11. https://doi.org/10.1186/s13643-021-01626-4 .
Fontaine G, Cossette S, Maheu-Cadotte MA, et al. Effect of implementation interventions on nurses’ behaviour in clinical practice: a systematic review, meta-analysis and meta-regression protocol. Syst Rev. 2019;8(1):305. https://doi.org/10.1186/s13643-019-1227-x .
Clarivate. EndNote X8 [Computer software]. https://endnote.com/product-details/x8/ . Accessed 20 Sept 2024.
Covidence. Covidence [Computer software]. https://www.covidence.org/ . Accessed 20 Sept 2024.
Sterne JA, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366. https://doi.org/10.1136/bmj.l4898
Sterne JA, Hernán MA, Reeves BC, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355 https://doi.org/10.1136/bmj.i4919
Cochrane. Review Manager Web (RevMan Web) Version 7.7.0 [Computer software]. https://revman.cochrane.org
McGuinness L, Higgins, JPT. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res Syn Meth. 2020:1–7. https://doi.org/10.1002/jrsm.1411
Guyatt G, Oxman AD, Akl EA, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94. https://doi.org/10.1016/j.jclinepi.2010.04.026 .
GRADEpro GDT: GRADEpro Guideline development tool [Software]. McMaster University and evidence prime. 2024. Available from gradepro.org .
Antonini M, Bellier-Teichmann T, O’Reilly L, et al. Effects of an educational intervention to strengthen humanistic practice on haemodialysis nurses’ caring attitudes and behaviours and quality of working life: a cluster randomised controlled trial. BMC Nurs. 2021;20(1):255. https://doi.org/10.1186/s12912-021-00729-6 .
Brady MC, Stott DJ, Weir CJ, et al. A pragmatic, multi-centered, stepped wedge, cluster randomized controlled trial pilot of the clinical and cost effectiveness of a complex Stroke Oral healthCare intervention pLan Evaluation II (SOCLE II) compared with usual oral healthcare in stroke wards. Int J Stroke. 2020;15(3):318–23. https://doi.org/10.1177/1747493019871824 .
Brennan K, Sanchez D, Hedges S, et al. A nurse-led intervention to reduce the incidence and duration of delirium among adults admitted to intensive care: a stepped-wedge cluster randomised trial. Aust Criti Care. 2023;36(4):441–8. https://doi.org/10.1016/j.aucc.2022.08.005 .
Chang Y-Y, Yu H-H, Loh E-W, Chang L-Y. The efficacy of an in-service education program designed to enhance the effectiveness of physical restraints. J Nurs Res. 2016;24(1):79–86. https://doi.org/10.1097/jnr.0000000000000092 .
Day T, Wainwright SP, Wilson-Barnett J. An evaluation of a teaching intervention to improve the practice of endotracheal suctioning in intensive care units. J Clin Nurs. 2001;10(5):682–96. https://doi.org/10.1046/j.1365-2702.2001.00519.x .
Article CAS PubMed Google Scholar
Hammersley VS, Elton RA, Walker S, Hansen CH, Sheikh A. Adolescent seasonal allergic rhinitis and the impact of health-care professional training: Cluster randomised controlled trial of a complex intervention in primary care. NPJ Prim Care Respir Med. 2014;24:14012. https://doi.org/10.1038/npjpcrm.2014.12 .
Happ MB, Sereika SM, Houze MP, et al. Quality of care and resource use among mechanically ventilated patients before and after an intervention to assist nurse-nonvocal patient communication. Heart & Lung. 2015;44(5):408-415. e2. https://doi.org/10.1016/j.hrtlng.2015.07.001 .
Hessig RE, Arcand LL, Frost MH. The effects of an educational intervention on oncology nurses’ attitude, perceived knowledge, and self-reported application of complementary therapies. Oncol Nurs Forum. 2004;31(1):71–8. https://doi.org/10.1188/04.Onf.71-78 .
Hödl M, Halfens RJ, Lohrmann C. Effectiveness of conservative urinary incontinence management among female nursing home residents—a cluster RCT. Arch Gerontol Geriatr. 2019;81:245–51. https://doi.org/10.1016/j.archger.2019.01.003 .
Hong SW, Ching TY, Fwng JPM, Seto WL. The employment of ward opinion leaders for continuing education in the hospital. Med Teach. 1990;12(2):209–17. https://doi.org/10.3109/01421599009006698 .
Johnston CC, Gagnon A, Rennick J, et al. One-on-one coaching to improve pain assessment and management practices of pediatric nurses. J Pediatr Nurs. 2007;22(6):467–78. https://doi.org/10.1016/j.pedn.2007.07.004 .
Lim SC, Mustapha FI, Aagaard-Hansen J, Calopietro M, Aris T, Bjerre-Christensen U. Impact of continuing medical education for primary healthcare providers in Malaysia on diabetes knowledge, attitudes, skills and clinical practices. Med Educ Online. 2020;25(1):1710330. https://doi.org/10.1080/10872981.2019.1710330 .
Lin PC, Chiang HW, Chiang TT, Chen CS. Pain management: evaluating the effectiveness of an educational programme for surgical nursing staff. J Clin Nurs. 2008;17(15):2032–41. https://doi.org/10.1111/j.1365-2702.2007.02190.x .
Michaels TK, Hubbartt E, Carroll SA, Hudson-Barr D. Evaluating an educational approach to improve pain assessment in hospitalized patients. J Nurs Care Qual. 2007;22(3):260–5. https://doi.org/10.1097/01.Ncq.0000277784.14310.66 .
Noordman J, van der Weijden T, van Dulmen S. Effects of video-feedback on the communication, clinical competence and motivational interviewing skills of practice nurses: a pre-test posttest control group study. J Adv Nurs. 2014;70(10):2272–83. https://doi.org/10.1111/jan.12376 .
O’Neill KL, Ross-Kerr JC. Impact of an instructional program on nurses’ accuracy in capillary blood glucose monitoring. Clin Nurs Res. 1999;8(2):166–78. https://doi.org/10.1177/10547739922158223 .
Pagaiya N, Garner P. Primary care nurses using guidelines in Thailand: a randomized controlled trial. Trop Med Int Health. 2005;10(5):471–7. https://doi.org/10.1111/j.1365-3156.2005.01404.x .
Reynolds SS, Woltz P, Keating E, et al. Results of the CHlorhexidine Gluconate Bathing implementation intervention to improve evidence-based nursing practices for prevention of central line associated bloodstream infections Study (CHanGing BathS): a stepped wedge cluster randomized trial. Implement Sci. 2021;16(1):45. https://doi.org/10.1186/s13012-021-01112-4 .
Rothschild JM, Keohane CA, Cook EF, et al. A controlled trial of smart infusion pumps to improve medication safety in critically ill patients. Crit Care Med. 2005;33(3):533–40. https://doi.org/10.1097/01.ccm.0000155912.73313.cd .
Schondelmeyer AC, Bettencourt AP, Xiao R, et al. Evaluation of an educational outreach and audit and feedback program to reduce continuous pulse oximetry use in hospitalized infants with stable bronchiolitis: a nonrandomized clinical trial. JAMA Netw Open. 2021;4(9):e2122826. https://doi.org/10.1001/jamanetworkopen.2021.22826 .
Seeley MA, Harding KG. The effects of education and training on clinical practice in wound healing. Int Wound J. 2008;5(5):660–4. https://doi.org/10.1111/j.1742-481X.2008.00519.x .
Segal G, Karniel E, Mahagna A, Kaa’dan F, Levi Z, Balik C. A nurse-guided, basal-prandial insulin treatment protocol for achieving glycaemic control of hospitalized, non-critically ill diabetes patients, is non-inferior to physician-guided therapy: a pivotal, nurse-empowerment study. International Journal of Mursing Practice. 2015;21(6):790–6. https://doi.org/10.1111/ijn.12292 .
Van de Steeg L, IJkema R, Langelaan M, Wagner C. Can an e-learning course improve nursing care for older people at risk of delirium: a stepped wedge cluster randomised trial. BMC Geriatr. 2014;14(1):1–8. https://doi.org/10.1186/1471-2318-14-69 .
Walsh TS, Kydonaki K, Antonelli J, et al. Staff education, regular sedation and analgesia quality feedback, and a sedation monitoring technology for improving sedation and analgesia quality for critically ill, mechanically ventilated patients: a cluster randomised trial. Lancet Respir Med. 2016;4(10):807–17. https://doi.org/10.1016/S2213-2600(16)30178-3 .
Woodcock AJ, Kinmonth A-L, Campbell MJ, Griffin SJ, Spiegal NM. Diabetes care from diagnosis: effects of training in patient-centred care on beliefs, attitudes and behaviour of primary care professionals. Patient Educ Couns. 1999;37(1):65–79. https://doi.org/10.1016/S0738-3991(98)00104-9 .
Morita T, Murata H, Kishi E, Miyashita M, Yamaguchi T, Uchitomi Y. Meaninglessness in terminally ill cancer patients: a randomized controlled study. J Pain Symptom Manage. 2009;37(4):649–58. https://doi.org/10.1016/j.jpainsymman.2008.04.017 .
Wald HL, Bandle B, Richard AA, Min SJ, Capezuti E. A Trial of electronic surveillance feedback for quality improvement at Nurses Improving Care for Healthsystem Elders (NICHE) hospitals. Am J Infect Control. 2014;42(10 Suppl):S250–6. https://doi.org/10.1016/j.ajic.2014.04.018 .
Bittner MJ, Rich EC, Turner PD, Arnold WH Jr. Limited impact of sustained simple feedback based on soap and paper towel consumption on the frequency of hand washing in an adult intensive care unit. Infect Control Hosp Epidemiol. 2002;23(3):120–6. https://doi.org/10.1086/502020 .
Charrier L, Allochis MC, Cavallo MR, Gregori D, Cavallo F, Zotti CM. Integrated audit as a means to implement unit protocols: a randomized and controlled study. J Eval Clin Pract. 2008;14(5):847–53. https://doi.org/10.1111/j.1365-2753.2008.01042.x .
Jansson MM, Syrjala HP, Ohtonen PP, Merilainen MH, Kyngas HA, Ala-Kokko TI. Simulation education as a single intervention does not improve hand hygiene practices: a randomized controlled follow-up study. Am J Infect Control. 2016;44(6):625–30. https://doi.org/10.1016/j.ajic.2015.12.030 .
Kaner E, Lock C, Heather N, McNamee P, Bond S. Promoting brief alcohol intervention by nurses in primary care: a cluster randomised controlled trial. Patient Educ Couns. 2003;51(3):277–84. https://doi.org/10.1016/s0738-3991(02)00242-2 .
Lau BD, Shaffer DL, Hobson DB, et al. Effectiveness of two distinct web-based education tools for bedside nurses on medication administration practice for venous thromboembolism prevention: a randomized clinical trial. PLoS One. 2017;12(8):e0181664. https://doi.org/10.1371/journal.pone.0181664 .
Article CAS PubMed PubMed Central Google Scholar
Magnan MA, Maklebust J. The effect of Web-based Braden Scale training on the reliability and precision of Braden Scale pressure ulcer risk assessments. J Wound Ostomy Continence Nurs. 2008;35(2):199–208. https://doi.org/10.1097/01.WON.0000313643.60117.b2 . discussion 209.
Muller-Staub M, Needham I, Odenbreit M, Lavin MA, van Achterberg T. Implementing nursing diagnostics effectively: cluster randomized trial. J Adv Nurs. 2008;63(3):291–301. https://doi.org/10.1111/j.1365-2648.2008.04700.x .
Rutherford-Hemming T, Kelsey NC, Grenig DL, Feliciano M, Simko L, Henrich CM. Multisite single-blinded randomized control study of transfer and retention of knowledge and skill between nurses using simulation and online self-study module. Simul Healthc. 2016;11(4):264–70. https://doi.org/10.1097/sih.0000000000000168 .
Wang L, Chen H, Yang L, Qian C, Sun D, Sun Y. Systematic training program for nursing home staff based on the concept of combination of medicine and care. Medicine. 2020;99(24):e20559. https://doi.org/10.1097/MD.0000000000020559 .
Jansson MM, Ala-Kokko TI, Ohtonen PP, Merilainen MH, Syrjala HP, Kyngas HA. Human patient simulation education in the nursing management of patients requiring mechanical ventilation: a randomized, controlled trial. Am J Infect Control. 2014;42(3):271–6. https://doi.org/10.1016/j.ajic.2013.11.023 .
Wang J, Wei L, Li H, et al. Effectiveness of a Game-Based Phone Application in Educating Health Care Workers on the Proper Use of Personal Protective Equipment. J Contin Educ Nurs. 2022;53(5):212–20. https://doi.org/10.3928/00220124-20220414-03 .
Tsai WP, Lin LY, Chang HC, Yu LS, Chou MC. The effects of the gatekeeper suicide-awareness program for nursing personnel. Perspect Psychiatr Care. 2011;47(3):117–25. https://doi.org/10.1111/j.1744-6163.2010.00278.x .
Carrico RM, Coty MB, Goss LK, LaJoie AS. Changing health care worker behavior in relation to respiratory disease transmission with a novel training approach that uses biosimulation. Am J Infect Control. 2007;35(1):14–9. https://doi.org/10.1016/j.ajic.2005.12.013 .
Kinsman L, Cooper S, Champion R, et al. The impact of web-based and face-to-face simulation education programs on nurses’ response to patient deterioration: a multi-site interrupted time series study. Nurse Educ Today. 2021;102: 104939. https://doi.org/10.1016/j.nedt.2021.104939 .
Chambers A, Chen C, Brown KA, et al. Virtual learning collaboratives to improve urine culturing and antibiotic prescribing in long-term care: controlled before-and-after study. BMJ Qual Saf. 2022;31(2):94–104. https://doi.org/10.1136/bmjqs-2020-012226 .
Fabre V, Pleiss A, Klein E, et al. A Pilot study to evaluate the impact of a nurse-driven urine culture diagnostic stewardship intervention on urine cultures in the acute care setting. Jt Comm J Qual Patient Saf. 2020;46(11):650–5. https://doi.org/10.1016/j.jcjq.2020.07.003 .
Hutchinson AM, Brotto V, Chapman A, Sales AE, Mohebbi M, Bucknall TK. Use of an audit with feedback implementation strategy to promote medication error reporting by nurses. J Clin Nurs. 2020;29(21–22):4180–93. https://doi.org/10.1111/jocn.15447 .
Jansson MM, Syrjala HP, Ohtonen PP, Merilainen MH, Kyngas HA, Ala-Kokko TI. Randomized, controlled trial of the effectiveness of simulation education: a 24-month follow-up study in a clinical setting. Am J Infect Control. 2016;44(4):387–93. https://doi.org/10.1016/j.ajic.2015.10.035 .
Happ MB, Sereika SM, Houze MP, et al. Quality of care and resource use among mechanically ventilated patients before and after an intervention to assist nurse-nonvocal patient communication. Heart Lung. 2015;44(5):408-415.e2. https://doi.org/10.1016/j.hrtlng.2015.07.001 .
Ivers N YS, Lacroix M, Brown KA, Antony J, Soobiah C, Simeoni M, Willis TA, Crawshaw J, Antonopoulou V, Meyer C, Solbak NM, Murray BJ, Butler E, Zahradnik M, Lepage S, Giltenane M, Carter MD, Fontaine G, Sykes M, Halasy M, Bazazo A, Seaton S, Canavan T, Alderson S, Reis C, Linklater S, Lalor A, Fletcher A, Gearon E, Jenkins H, Wallis JA, Grobler L, Beccaria L, Cyril S, Rozbroj T, Han JC, Xu AXT, Wu K, Rouleau G, Shah M, Konnyu K, Colquhoun H, Presseau J, O'Connor D, Lorencatto F, Grimshaw JM,. Audit and feedback: effects on professional practice and healthcare outcomes. Cochrane Database Syst Rev. 2024.
Michie S, van Stralen MM, West R. The behaviour change wheel: a new method for characterising and designing behaviour change interventions. Implement Sci. 2011;6:42. https://doi.org/10.1186/1748-5908-6-42 .
Squires JE, Sullivan K, Eccles MP, Worswick J, Grimshaw JM. Are multifaceted interventions more effective than single-component interventions in changing health-care professionals’ behaviours? An overview of systematic reviews. Implement Sci. 2014;9:152. https://doi.org/10.1186/s13012-014-0152-6 .
Baker R, Camosso-Stefinovic J, Gillies C, et al. Tailored interventions to address determinants of practice. Cochrane Database Syst Rev. 2015;2015(4):CD005470. https://doi.org/10.1002/14651858.CD005470.pub3 .
Connor L, Dean J, McNett M, et al. Evidence-based practice improves patient outcomes and healthcare system return on investment: findings from a scoping review. Worldviews Evid Based Nurs. 2023;20(1):6–15. https://doi.org/10.1111/wvn.12621 .
Lovero KL, Kemp CG, Wagenaar BH, et al. Application of the Expert Recommendations for Implementing Change (ERIC) compilation of strategies to health intervention implementation in low- and middle-income countries: a systematic review. Implement Sci. 2023;18(1):56. https://doi.org/10.1186/s13012-023-01310-2 .
Download references
Acknowledgements
The authors wish to acknowledge the contribution of Jérémie Blondin for the development of search strategies and the search in bibliographical databases. We thank Ariane Ballard for contributing to study selection. We thank the individuals who responded to requests for additional data, including Jens Abraham, Patrick Akande, Marvin J. Bittner, Ian Blanco Mavillard, Nicolle P. G. Boumans, Marian C. Brady, Diane L. Carroll, Andrea Chaplin, Lorena Charrier, Francine M. Cheater, Lynn Chenoweth, Yeu-Hui Chuang, Lorenzo Cohen, Kelly Jo Cone, Susan Cortez, J. Randall Curtis, Barbara Davies, Tina Day, Marlies de Rond, Dennis de Ruijter, Helen Edwards, Mohamed Elzeky, Ruth Engelberg, David Evans, Valeria Fabre, Tobias Filmer, Christopher R. Friese, Marjorie Funk, Matthew Bidwell Goetz, Salla Grommi, Mary Beth Happ, Michael Hendryx, Manuela Hödl, Anita Huis, Alison Hutchinson, Yueh-Juan Hwu, Ali Khani Jeihooni, Céleste Johnston, Eileen F. S. Kaner, Zahra Karimian, Kristina H. Karvinen, Sedigheh Khanjari, Mahnaz Khatiban, Serena Koh, Sascha Köpke, Ruth Kleinpell, Una Kyriacos, Jan van Lieshout, Li-Chan Lin, Elizabeth Manias, Edward R. Marcantonio, Gabriele Meyer, Sandy Middleton, Tatsuya Morita, Janneke Noordman, Mary Patricia Nowalk, Jane Ogden, Christine Paul, James A. Rankin, Marilyn Rantz, Susan M. Ray, Staci S. Reynolds, Young Sook Roh, Jeffrey M. Rothschild, Reza Sadeghi, Trygve Johannes Lereim Sævareid, Parvin Mangolian Shahrbabaki, Davide Sisti, Wilma ten Ham-Baoyi, Sousan Valizadeh, Maritta Välimäki, Ayse Kacaroglu Vicdan, Thomas von Lengerke, Laura Wagner, Timothy Walsh, Marcia Weaver, Chistopher Weir, and Carla Zotti.
GF was supported by a Banting Postdoctoral Fellowship (#202010BPF-453986–255367) from the Canadian Institutes of Health Research (CIHR), and a Junior 1 Research Scholar Award from the Fonds de recherche du Québec – Santé (FRQ-S). This project is supported by a project grant from the Quebec Health Research Fund (FRQ-S) and the Réseau de recherche en interventions en sciences infirmières du Québec/Quebec Network on Nursing Intervention Research (RRISIQ).
Author information
Authors and affiliations.
Ingram School of Nursing, Faculty of Medicine and Health Sciences, McGill University, 680 Rue Sherbrooke West, 18Th Floor, Office 1812, Montréal, QC, H3A 2M7, Canada
Guillaume Fontaine, Charlene Weight, Sonia A. Castiglione, Meagan Mooney & Sonia Semenic
Centre for Clinical Epidemiology, Lady Davis Institute for Medical Research, Sir Mortimer B. Davis Jewish General Hospital, CIUSSS West-Central Montreal, 3755 Chem. de La Côte-Sainte-Catherine, Montréal, QC, H3T 1E2, Canada
Guillaume Fontaine
Centre for Nursing Research, Sir Mortimer B. Davis Jewish General Hospital, CIUSSS West-Central Montreal, 3755 Chem. de La Côte-Sainte-Catherine, Montréal, QC, H3T 1E2, Canada
Guillaume Fontaine & Nikolas Argiropoulos
Centre for Implementation Research, Methodological and Implementation Research Program, Ottawa Hospital Research Institute, 501 Smyth Road, Ottawa, ON, K1H 8L6, Canada
Faculty of Nursing, Université de Montréal, 2375 Chemin de La Côte-Sainte-Catherine, Montréal, QC, H3T 1A8, Canada
Billy Vinette, Marc-André Maheu-Cadotte, Marie-France Deschênes, Tanya Mailhot, Patrick Lavoie & Sylvie Cossette
Research Centre of the Centre Hospitalier de L’Université de Montréal, 900 Saint Denis St, Montreal, QC, H2X 0A9, Canada
Billy Vinette & Gabrielle Chicoine
Division of Child and Adolescent Health, Department of Pediatrics, Columbia University Vagelos College of Physicians and Surgeons and NewYork-Presbyterian Morgan Stanley Children’s Hospital, 3659 Broadway, New York, NY, 10032, USA
Andréane Lavallée
Centre de Recherche Interdisciplinaire en Réadaptation du Montréal Métropolitain, Institut de Réadaptation Gingras-Lindsay-de-Montréal, 6363 Hudson Rd, Montréal, QC, H3S 1M9, Canada
Marie-France Deschênes
CHU de Québec-Université Laval Research Centre, 1050 Chemin Sainte-Foy, Québec City, QC, G1S 4L8, Canada
Alexandra Lapierre & Marie-Pierre Gagnon
Research Institute of the McGill University Health Centre, 2155 Guy St, Montreal, QC, H3H 2L9, Canada
Sonia A. Castiglione & Sonia Semenic
Knowledge Translation Program, Li Ka Shing Knowledge Institute, St. Michael’s Hospital, Unity Health Toronto, 38 Shuter St, Toronto, ON, M5B 1A6, Canada
Gabrielle Chicoine
Department of Nursing, Université du Québec en Outaouais, 283, Boulevard Alexandre-Taché, Gatineau, QC, J8X 3X7, Canada
Geneviève Rouleau
Women’s College Hospital Institute for Health System Solutions and Virtual Care, Women’s College Hospital, 76 Grenville St, Toronto, ON, M5G 1N8, Canada
Health Services Research Unit, School of Medicine, Medical Sciences and Nutrition, University of Aberdeen, Health Sciences Building Foresterhill, Aberdeen, AB25 2ZD, UK
Kristin Konnyu
School of Nursing, Dalhousie University, 5869 University Ave, Halifax, NS, B3H 4R2, Canada
Christine E. Cassidy
IWK Health, 5980 University Ave, Halifax, NS, B3K 6R8, Canada
Montreal Heart Institute Research Centre, 5000 Bélanger, Montréal, QC, H1T 1C8, Canada
Tanya Mailhot, Patrick Lavoie & Sylvie Cossette
Centre Intégré de Santé et de Services Sociaux de Chaudière-Appalaches, 143, Rue Wolfe, Lévis, QC, G6V 3Z1, Canada
Catherine Pépin
Faculty of Nursing, Université Laval, Pavillon Ferdinand-Vandry, 1050, Avenue de La Médecine, Québec City, QC, G1V 0A6, Canada
Marie-Pierre Gagnon
Nursing Research Institute, St Vincent’s Health Network Sydney, St Vincent’s Hospital Melbourne and the Australian Catholic University, 390 Victoria St, Level 5 deLacy Building, Darlinghurst, NSW, 2010, Australia
Nicola Straiton & Sandy Middleton
School of Nursing, Midwifery and Paramedicine, Australian Catholic University, 40 Edward Street, North Sydney, Sydney, NSW, 2060, Australia
Sandy Middleton
You can also search for this author in PubMed Google Scholar
Contributions
GF conceptualized the study, developed the research questions, and defined the scope of the review. GF, in collaboration with a Research Librarian, designed and ran the search strategies. Title and abstract screening were performed by GF, BV, MAMC, ALav, MFD, ALap, GC, GR and CP. The full text review was carried out by GF, BV, MAMC, ALav, MFD, ALap, GC, GR, CEC and CP. Data extraction and risk of bias assessment were conducted by GF, BV, CW, MAMC, ALav, MFD, ALap, SAC, GC, GR, NA, MM, CEC, CP, TM and PL. GF, BV, CW, and NA managed the data cleaning and performed the meta-analyses, which were reviewed by KK. GF, BV and CW prepared the tables and figures, while GF and CW led the narrative synthesis and drafted the manuscript. KK, SC, MPG, SS, NS and SM provided critical input into the organization, analysis, and interpretation of the results. All authors read and approved the final manuscript.
Corresponding author
Correspondence to Guillaume Fontaine .
Ethics declarations
Ethics approval and consent to participate.
Not applicable.
Consent for publication
Competing interests.
The authors declare that they have no competing interests.
Additional information
Publisher’s note.
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Supplementary material 1., supplementary material 2., supplementary material 3., supplementary material 4., supplementary material 5., supplementary material 6., supplementary material 7., supplementary material 8., supplementary material 9., supplementary material 10., rights and permissions.
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/ .
Reprints and permissions
About this article
Cite this article.
Fontaine, G., Vinette, B., Weight, C. et al. Effects of implementation strategies on nursing practice and patient outcomes: a comprehensive systematic review and meta-analysis. Implementation Sci 19 , 68 (2024). https://doi.org/10.1186/s13012-024-01398-0
Download citation
Received : 04 July 2024
Accepted : 13 September 2024
Published : 30 September 2024
DOI : https://doi.org/10.1186/s13012-024-01398-0
Share this article
Anyone you share the following link with will be able to read this content:
Sorry, a shareable link is not currently available for this article.
Provided by the Springer Nature SharedIt content-sharing initiative
- Implementation strategies
- Quality improvement
- Knowledge translation strategies
- Nursing practice
- Professional practice
- Clinical practice
- Healthcare professional behavior
- Patient outcomes
Implementation Science
ISSN: 1748-5908
- Submission enquiries: Access here and click Contact Us
- General enquiries: [email protected]
Log in using your username and password
- Search More Search for this keyword Advanced search
- Latest content
- Current issue
- Write for Us
- BMJ Journals More You are viewing from: Google Indexer
You are here
- Volume 14, Issue 3
- What is a systematic review?
- Article Text
- Article info
- Citation Tools
- Rapid Responses
- Article metrics
- Jane Clarke
- Correspondence to Jane Clarke 4 Prime Road, Grey Lynn, Auckland, New Zealand; janeclarkehome{at}gmail.com
https://doi.org/10.1136/ebn.2011.0049
Statistics from Altmetric.com
Request permissions.
If you wish to reuse any or all of this article please use the link below which will take you to the Copyright Clearance Center’s RightsLink service. You will be able to get a quick price and instant permission to reuse the content in many different ways.
A high-quality systematic review is described as the most reliable source of evidence to guide clinical practice. The purpose of a systematic review is to deliver a meticulous summary of all the available primary research in response to a research question. A systematic review uses all the existing research and is sometime called ‘secondary research’ (research on research). They are often required by research funders to establish the state of existing knowledge and are frequently used in guideline development. Systematic review findings are often used within the healthcare setting but may be applied elsewhere. For example, the Campbell Collaboration advocates the application of systematic reviews for policy-making in education, justice and social work.
Systematic reviews can be conducted on all types of primary research. Many are reviews of randomised trials (addressing questions of effectiveness), cross-sectional studies (addressing questions about prevalence or diagnostic accuracy, for example) or cohort studies (addressing questions about prognosis). When qualitative research is reviewed systematically, it may be described as a systematic review, but more often other terms such as meta-synthesis are used.
Systematic review methodology is explicit and precise and aims to minimise bias, thus enhancing the reliability of the conclusions drawn. 1 , 2 The features of a systematic review include:
■ clear aims with predetermined eligibility and relevance criteria for studies;
■ transparent, reproducible methods;
■ rigorous search designed to locate all eligible studies;
■ an assessment of the validity of the findings of the included studies and
■ a systematic presentation, and synthesis, of the included studies. 3
The first step in a systematic review is a meticulous search of all sources of evidence for relevant studies. The databases and citation indexes searched are listed in the methodology section of the review. Next, using predetermined reproducible criteria to screen for eligibility and relevance assessment of titles and the abstracts is completed. Each study is then assessed in terms of methodological quality.
Finally, the evidence is synthesised. This process may or may not include a meta-analysis. A meta-analysis is a statistical summary of the findings of independent studies. 4 Meta-analyses can potentially present more precise estimates of the effects of interventions than those derived from the individual studies alone. These strategies are used to limit bias and random error which may arise during this process. Without these safeguards, then, reviews can mislead, such that we gain an unreliable summary of the available knowledge.
The Cochrane Collaboration is a leader in the production of systematic reviews. Cochrane reviews are published on a monthly basis in the Cochrane Database of Systematic Reviews in The Cochrane Library (see: http://www.thecochranelibrary.com ).
- Antman EM ,
- Kupelnick B ,
- Higgins JPT ,
Competing interests None.
Read the full text or download the PDF:

IMAGES
VIDEO
COMMENTS
A systematic literature review has the same structure as an original research article: TITLE: The systematic review title should indicate the content. The title should reflect the research question, however it should be a statement and not a question. ... Price B. Guidance on conducting a literature search reviewing mixed literature. Nursing ...
As the systematic review advances, the subsequent crucial steps involve data extraction from the studies included. ... How to do a systematic literature review in nursing: a step-by-step guide. [Google Scholar] 9. Utilization of the PICO framework to improve searching PubMed for clinical questions. Schardt C, Adams MB, Owens T, Keitz S, Fontelo ...
Before undertaking a systemic review, a research question should first be formulated (Bashir and Conlon, 2018). There are a number of tools/frameworks (Table 1) to support this process, including the PICO/PICOS, PEO and SPIDER criteria (Bowers et al, 2011). These frameworks are designed to help break down the question into relevant subcomponents and map them to concepts, in order to derive a ...
A solid understanding of the systematic review process can be of benefit to nurses that carry out such reviews, and for those who make decisions based on them. An overview of the main steps involved in carrying out a systematic review is presented, including some of the common tools and frameworks utilised in this area.
Aims: This paper aims to provide a systematic review of the international literature, to synthesise knowledge and explore factors that influence nurses' adherence to patient-safety principles. Methods: Electronic databases in English, Norwegian, and Finnish languages were searched, using appropriate keywords to retrieve empirical articles ...
Nurses' continuing professional development (CPD) improves the quality of nursing care, patients' safety, nurses' satisfaction and healthcare costs. However, evidence has shown that nurses do not always participate in their CPD and that CPD does not always address nurses' real needs. To examine this …
In many countries nursing practice associated with formulating nursing care plans has not been thoroughly explained in nursing literature. Standardized nursing language (SNL) is an established of terms used to label the clinical judgments involved in nursing assessment (Rabelo-Silva et al., 2017).Attempts to introduce SNL and capture the impacts are important to increase the visibility of ...
CONCLUSION. Siddaway 16 noted that, "The best reviews synthesize studies to draw broad theoretical conclusions about what the literature means, linking theory to evidence and evidence to theory" (p. 747). To that end, high quality systematic reviews are explicit, rigorous, and reproducible. It is these three criteria that should guide authors seeking to write a systematic review or editors ...
Background Implementation strategies targeting individual healthcare professionals and teams, such as audit and feedback, educational meetings, opinion leaders, and reminders, have demonstrated potential in promoting evidence-based nursing practice. This systematic review examined the effects of the 19 Cochrane Effective Practice and Organization Care (EPOC) healthcare professional-level ...
A high-quality systematic review is described as the most reliable source of evidence to guide clinical practice. The purpose of a systematic review is to deliver a meticulous summary of all the available primary research in response to a research question. A systematic review uses all the existing research and is sometime called 'secondary research' (research on research). They are often ...